Case Study: How the University of Illinois Craniofacial Center Is Successfully Correcting Facial Asymmetry With Surgical Guides and Postoperative Masks
Facial asymmetry can occur for a number of reasons including genetics, injury, or disease. One common solution to severe facial asymmetry is to strategically inject the patient’s own adipose tissue into low points of the face to restore volume, also known as autologous fat grafting. This procedure must be done with the utmost precision in order to bring balance back to the face and leave patients with satisfactory results.
Clinical outcomes of this procedure are generally good, but vary based on the surgeon’s ability to judge how much and where fat should be injected. Historically, surgeons have used clinical photos to plan for these procedures, but are limited by their 2D nature. The introduction of 3D medical imaging has allowed for more precise and accurate pre-surgical planning and improved patient outcomes.
Clinicians at the University of Illinois Craniofacial Center have taken an innovative approach to improving the precision and accuracy of analogous fat grafting procedures: patient-specific surgical guides and postoperative masks printed using Formlabs Surgical Guide Resin and Clear Resin. The customized surgical guides serve to define volumetric differences between the affected and the unaffected sides of the patient’s face, aiding the surgeon's judgment of how much fat to harvest, and where to inject it. The postoperative masks are used after surgery to evaluate the success of the procedure and the resulting facial symmetry.
Step-By-Step
Image Acquisition
The University of Illinois Craniofacial Center begins their procedure with digital photographs and a 3D scan of the patient’s facial anatomy. Cone beam computed tomography is captured for each patient using an iCAT scanner.
Segmentation
These 3D images are then imported into Mimics, a medical imaging software by Materialise. Using Mimics, the face is separated from the surrounding anatomy, and the model is saved in STL format.
Selection of Facial Landmarks
These STL files are imported into ZBrush, a digital sculpting software, and soft tissue landmarks are identified. Soft tissue landmarks are used to define the areas of interest on the unaffected side of the face, and indicate what areas should be replicated on the affected side. The nose and chin are included in this selection to aid with the repeated placement of the devices on the patient.

Selection of the area of interest on the unaffected side of the face.
Postoperative Mask Design
Once the unaffected area is defined, that area is mirrored onto the affected side of the face to simulate symmetry. This geometry is then assigned a 1.5 mm thickness to create a solid part and saved as a STL.

Mirroring of the unaffected area onto the affected area with a 1.5 mm thickness. This model will later serve as postoperative reference for the evaluation of surgical success.
Surgical Guide Design
To create the surgical guide, the affected side of the face is analyzed to determine what areas are lacking volume and symmetry. These landmarks are marked using the same processes as are used on the unaffected side. Similar to the unaffected side, this area is extruded to a 1.5 mm thickness.
The mirrored model of the unaffected side is overlaid on the model of the affected side. These two models are digitally fused to create a surgical guide with a container (gap between the affected and unaffected halves) that highlights the volumetric differences between the two halves of the face. This fused model is saved as an STL.

Mirroring of the unaffected area onto the affected area.

Fusion of the affected and unaffected areas to create a surgical guide that highlights areas of asymmetry and volumetric differences.
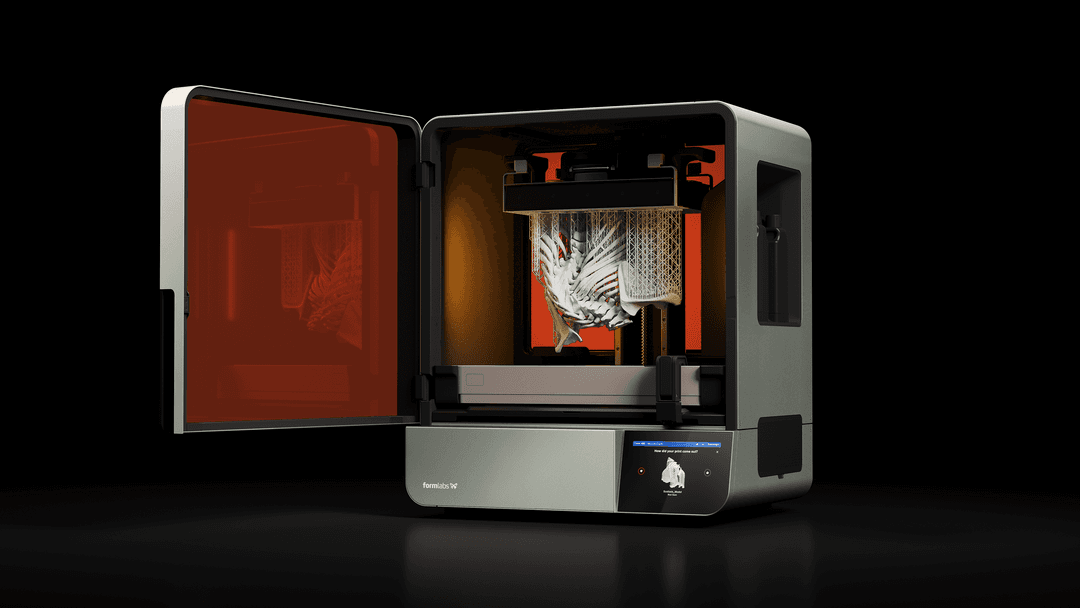
Printing and Post-Processing
Both the surgical guide and postoperative mask are uploaded into PreForm for print preparation, and printed using Surgical Guide Resin and Clear Resin respectively. Supports are removed and all parts are post-processed according to Formlabs’ Form Wash and Form Cure guidelines.

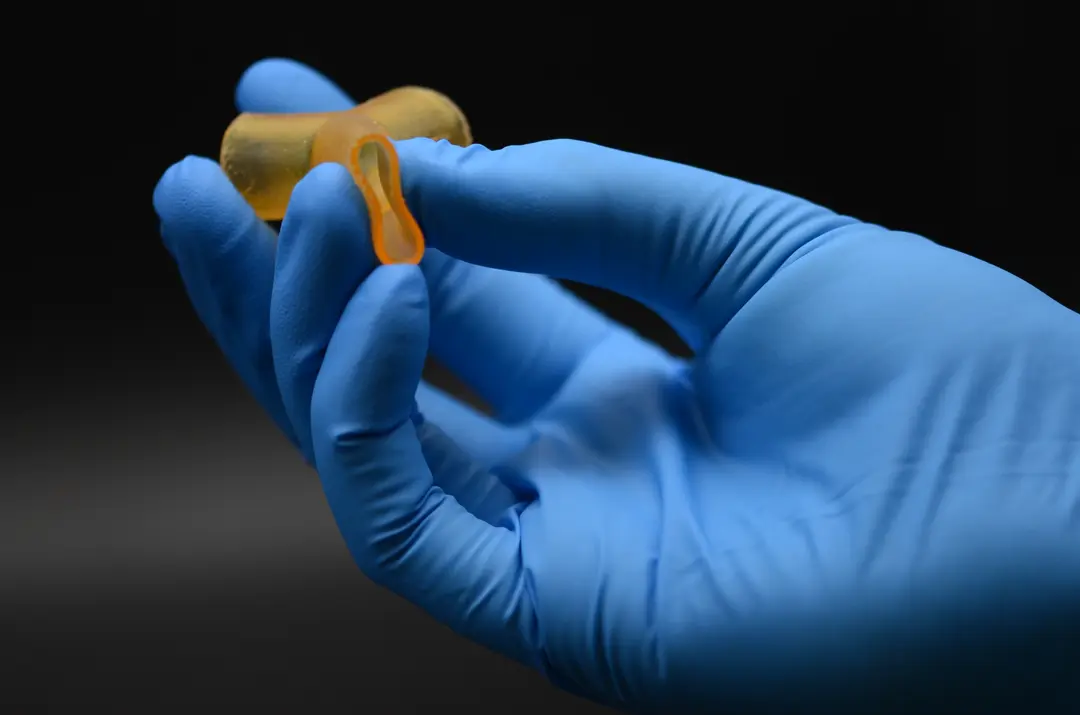
Postoperative mask printed in Clear Resin.
On the surgical guide, the exact amount of deficit is calculated in cubic centimeters (cc) by filling the container portions of the guide with water and measuring the amount it holds. This volume indicates to the surgeon exactly how much autologous fat needs to be harvested. Areas of volumetric deficit are marked directly on the part with a marker, and perforated to create through-holes in the areas where fat will need to be injected to restore symmetry.

Surgical guide with markings and perforations indicating areas of volumetric deficit.

BioMed Resin Swatches
Each BioMed Resin swatch features embossed and debossed designs, 0.5-2.0 mm cutout thicknesses, as well as regulatory information unique to that resin.
Sterilization and Surgical Technique
The surgical guides are sterilized according to Formlabs’ sterilization guidelines. The sterilized guides are taken into the operating room (OR) and placed against the affected anatomy. Perforations in the surgical guides help the surgeons mark the locations where fat should be injected directly on the patient with a skin marker. The surgical guide is removed and fat is injected in the marked areas in the exact volumes previously determined by measuring the volume of the guide. The postoperative mask is placed on the patient’s affected side after surgery to verify the appropriate placement of the injections.

The surgical guide being used in the OR to guide the placement of autologous fat injections.

Preoperative (top) and postoperative (bottom) view of a pediatric patient using the postoperative mask to validate the appropriate placement of fat injections.

3D Printing Applications for Hospitals and Patient-Specific Procedures
This report looks at five different ways the recent adoption of affordable in-house printing is impacting hospital and device manufacturers.
Outcomes
This method of strategically placing autologous fat using a patent-specific surgical guide has demonstrated 80-100% accuracy between the preoperative estimate of volumetric deficit and the amount injected in the operating room. Through this work, the University of Illinois Craniofacial Center has demonstrated that there are advantages to introducing a digital workflow to autologous fat grafting procedures and reducing reliance on surgeon intuition. In their peer-reviewed article in The Journal of Craniofacial Surgery, the team states “The value-added efficiencies introduced by this innovative technique present a difficult argument for not utilizing these advanced digital techniques for both preoperative planning and intraoperative guidance during fat grafting and verification of the successful application at the conclusion of the procedure.” More details about this procedure and its outcomes can be found in their article titled Virtual Surgical Planning and Three-Dimensional Printed Guide for Soft Tissue Correction in Facial Asymmetry.

Preoperative (left), frontal postoperative (middle), and coronal postoperative (right) views of a pediatric patient one week post-treatment.

Preoperative (left), frontal postoperative (middle), and coronal postoperative (right) views of an adult patient one week post-treatment.
Conclusion
The University of Illinois Craniofacial Center has demonstrated advances in preoperative planning, intraoperative decision-making, and postoperative care using patient-specific 3D printing.
Learn more about how Formlabs’ ecosystem can be used to improve patient outcomes, find out what biocompatible material is best fit for your application in our BioMed Materials white paper, or contact our team to discuss your specific application.