Treatment of Pediatric Vaginal Rhabdomyosarcoma With the Use of a Real-time Tracked Custom Applicator
Introduction: “Vaginal botryoides rhabdomyosarcoma (RMS) presents with an intraluminal mass. Treatment includes multi-agent chemotherapy and local control with organ-preserving surgery or radiation… commercially available vaginal cylinders are difficult to utilize in pediatric cases given that standard sizes are too large and are limited in their ability to dose optimize away from critical pediatric structures including the cervix and ovaries…. Compared to single-channel vaginal cylinders (SCVCs), multi-channel vaginal cylinders (MCVCs) improve target coverage and organ at risk (OAR) sparing thanks to the increased dose modulation capacity provided by the peripheral channels. The ability to adequately shape the dose distribution is of paramount importance in the setting of pediatric vaginal RMS….
In this work, we report on the design, quality assurance and clinical use of a custom MR/CT-compatible MCVC made of an FDA-approved, biocompatible material. We also describe an in-house real-time optical tracking system used for applicator position monitoring during treatment delivery.”
Materials and Methods:
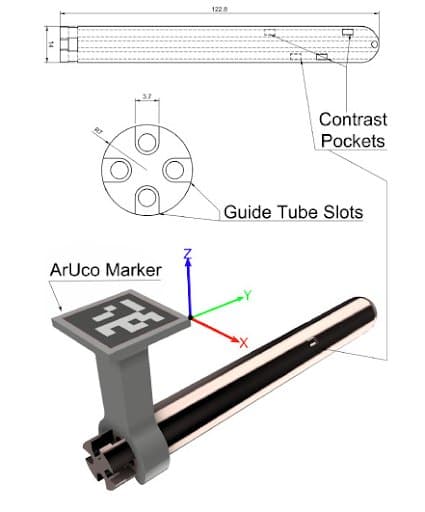
“Surgical resection was performed with residual microscopic positive margins… for a 4-year-old with vaginal botryoides rhabdomyosarcoma.” The patient “underwent MR-simulation with a custom 3D printed biocompatible resin cylinder with four channels to ensure dose optimization capability. A total of four identifier regions were designed into the applicator in order to utilize these for MR-visualization and real-time tracking. A biocompatible 3D printed cylinder was designed to meet dose objectives using an MR and CT compatible material. 3D slicer was required for real-time tracking during treatment.”
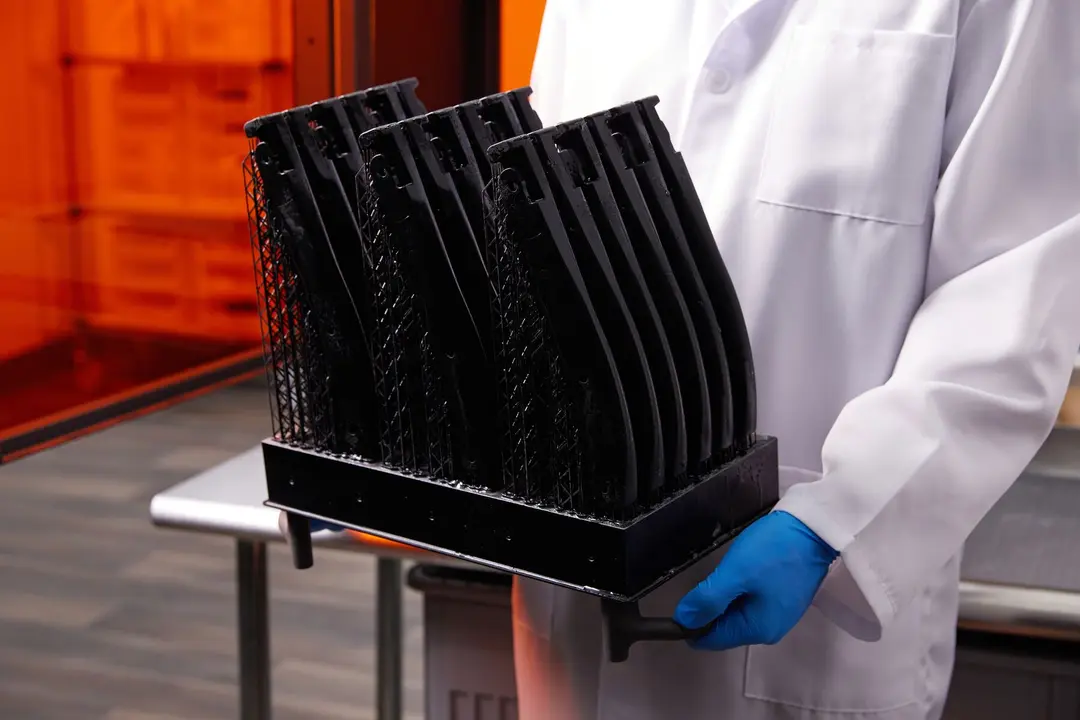
“The applicator was 3D printed using the biocompatible Dental-LT resin (Formlabs Inc., Sommerville, MA, USA). Dental LT Clear is a Class IIa CE-certified long-term (>30 days) biocompatible photopolymer resin that is typically used for intraoral applications.”
Results: “Based on MR simulation, a treatment plan was created with dose differentials in the area of prior surgery versus normal vaginal tissue. Creation of a low dose CT scan on a mobile CT allowed CT visualization of the applicator for verification. Treatment was administered under the use of a real-time optical tracking with rotational and depth adjustments monitored.”
“A video clip showing the entire real-time tracking workflow can be seen here: https://www.youtube.com/watch?v=3mj3AyjhYNc.”
“MCVC reduced OAR doses by up to 29% (compared to SCVC)”
Discussion: “We are the first to report on a custom 3D printed MR-compatible MCVC applicator with MR-fiducial pockets and optical tracking.
We selected the Dental-LT resin due to its biocompatibility, durability and the ability to 3D print this material within our institution, and because of the need to have image-guidance with both MR and CT. To implement this applicator for clinical use [we] conducted a validation of applicator visibility on MR and CT imaging and determined the radiation attenuation properties relative to water. Our novel applicator embedded MR-/CT-pockets filled with lubricant gel used as imaging fiducials that enable localization of the applicator in addition to its orientation which is an important degree of freedom with MCVCs….
The American College of Radiology practice guidelines report suggests a limit of 25 mGy dose for children, our methodology resulted in significantly lower dose than threshold (∼20 fold reduction).”
Conclusion: “This advanced integration of 3D printed MR and CT biocompatible material, with unique design features consistent with a multi-channel vaginal cylinder, and incorporation of real-time optical tracking ensured that no positional changes were required, allowed successful treatment with differential dosing for a post-operative pediatric vaginal rhabdomyosarcoma patient.”
Evaluation of a New Bi-valve Vaginal Speculum Applicator Design for Gynecologic Interstitial Brachytherapy
Purpose: “High-dose-rate (HDR) interstitial brachytherapy (ISBT) has been used in definitive gynecologic radiotherapy in patients with advanced cervical carcinoma. Significant improvements in survival have been reported with the addition of image guidance. Excellent clinical outcomes have been achieved with HDR ISBT using computed tomography (CT)-guided catheter placement for gynecologic cancer patients, and we routinely perform this procedure at our institution….
After CT images are acquired to evaluate the initial catheter position, catheter adjustment and additional catheter implantation are performed… To identify the appropriate location of additional needles, both insertion points and directions of additional needles are determined while confirming the positional relationship between catheters by direct visualization. However, in this situation, the conventional vaginal fornix applicator does not have visible insertion points due to its placement within the vagina….
To address this problem, we designed a bi-valve vaginal speculum high-dose-rate (HDR) interstitial gynecologic brachytherapy applicator. This allows for both a direct view of the cervix and image-guided brachytherapy applicator placement. The purpose of this study was to assess the validity of the new applicator.”
Materials and Methods: “A novel brachytherapy applicator was designed to have a shape similar to a bi-valve vaginal speculum, which allows the vaginal cavity to be opened and allows for a clear view of the cervix” It was produced on a Form 2 printer, “coupled with synergistic biocompatible resin (Dental SG Resin; Formlabs, Inc.), which is certified to comply with the international standards for class I biocompatibility, International Organization for Standardization (ISO) standard 10993-1.”
The print settings and orientation of the speculum applicator (not shown here) was set in PreForm.
“It is important to verify whether a new applicator can provide a pear-shaped dose distribution equivalent to that with a conventional tandem/ovoid applicator.
To compare the new and conventional applicator planning, we evaluated treated volume (including the dimensions of the 100% isodose volume), the dose-volume histogram (DVH) for a hypothetical cervix, and the dose points of organs at risk (OARs)...”
Results and Discussion: “No CT artifacts were visible inside the speculum applicator. The mean radiodensity of the Dental SG resin was 118 HU (standard deviation: 10 HU)...
The results showed that the difference in dosage between the vaginal speculum brachytherapy applicator and the intracavitary brachytherapy applicator was minimal in a clinical setting. There was a minimal difference in the dimensions of the 100% isodose volume… the treatment volumes overlapped, including the higher-dose volumes….
In this study, the validity of the new applicator was verified by comparison of the pear-shaped isodose distribution. Our novel ISBT applicator is combined with an intracavitary applicator; hence, it should be considered an advanced intracavitary applicator. Radiation oncologists will be able to exploit the direct view capability of our applicator to improve the conventional pear-shaped dose distribution, via use of additional interstitial needle applicators, thus enhancing target coverage.”
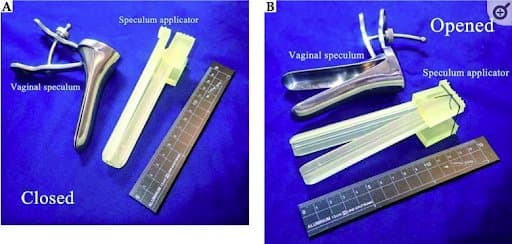
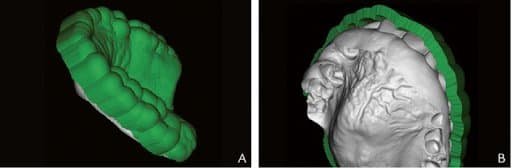
“The 3D-printed speculum applicator after polymerization. Each partially cylindrically shaped blade has a hinge structure, similar to that of the vaginal speculum. The applicator is shown with both blades closed (A), which facilitates its insertion, and opened (B), to allow a direct view of the cervix to be obtained. During implantation (B), the blades of the 3D-printed speculum applicator can be spread transversely to 35-mm wide, and then fixed via a black thread fed through the groove to maintain the applicator in an open position”
Conclusion: “We designed a novel vaginal speculum applicator with needle insertion holes for combined intracavitary and interstitial GYN HDR brachytherapy. Our speculum applicator, which allows for combined observation of the cervix through direct and imaging views for accurate catheter positioning and is produced using a 3D printer with biocompatible resin, can reproduce a conventional pear-shaped dose distribution. Our current clinical practice will use this applicator, which can improve patient treatment results.”
Individual 3-Dimensional Printed Mold for Treating Hard Palate Carcinoma With Brachytherapy: A Clinical Report
Introduction: “To increase local tumor control, high-dose-rate interventional brachytherapy (HDR-IRT) with custom molds is used for some head and neck cancer sites, especially in the oral cavity. It delivers a higher radiation dose locally and reduces the irradiated area, thus efficiently treating superficial tumors; it is associated with low toxicity and excellent cosmesis….
The [conventional] mold room experience which the patient must undergo is rarely well tolerated, particularly for a face shell. Furthermore, handmade custom molds are difficult to make for small area lesions, those with irregular surface contours, or those in difficult anatomic sites which need multiplane and multidirection catheter geometries. Three-dimensional (3D) printing may offer a solution for these difficulties. Automation could reduce fabrication time compared with hand molding, and computer optimization of catheter positions could improve dosimetry….
This clinical report describes the use of a 3-dimensional (3D) printer to create an individual mold for delivering
high-dose-rate interventional radiotherapy for hard palate cancer.”
Materials and Methods: “The maxillary teeth and palate were scanned with an intraoral scanner (3Shape TRIOS 3). The scan was transformed into a mesh using the standard tessellation language (STL) format and aligned with Digital Imaging and Communications in Medicine (DICOM) computed tomography (CT) images using free Blue Sky Plan 4 planning software. A mold was generated by tracing a guideline around the gingival margins of the maxillary teeth and palate on the scan mesh in accordance with established parameters. All data were imported into computer-aided design (CAD) software. For this patient, 3 parallel 2.2-mm-diameter ducts were placed 10 mm from each other in the mold mesh….
This palate radiotherapy mold was produced by the Formlabs Form 2, 3D printer by using stereolithography technology and Formlabs Dental SG Resin, which is approved for use in dental biomedical devices. After the mold was inserted into the patient's mouth, a CT scan (2.5-mm slices) evaluated its placement and was used for treatment planning.”
Mold generation. A, Maxillary left panel. External surface of mold showing maxillary teeth, hard palate. B, Intaglio surface of mold showing lesion.
Results: “The intended treatment was to deliver ≥95% of the prescribed dose to the planning target volume (PTV), accepting 90% as satisfactory. The mold was ready for use within 5 hours. The 3D-printed mold provided effective dose coverage in the PTV with V95%=99.01%. HDR-IRT treatment using the 3D mold was well tolerated with no patient discomfort reported.”
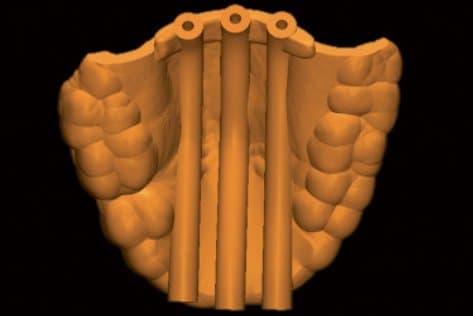
Catheter ducts
Discussion: ”As far as the authors are aware, this is the first description of a process for creating an HDR-IRT 3D printed mold to treat intraoral carcinoma. This patient's outcome suggests that because individual 3D printed molds have the potential to replace commercially available materials with handmade molds, their use may well become standard for oral cancer treatment with HDR-IRT…. The immediate advantage of intraoral scanning with a contactless surface scanner and 3D-printed mold was that patient discomfort was greatly reduced. The process is much less invasive and less time-consuming than a conventional polymeric dental impression and a scanned cast. The intraoral scanner did not contact the lesion and reduced the number of steps that could lead to errors. Because catheter positioning and number were based on the patient's CT data, CT-based planning ensured tumor coverage. Treatment was efficiently delivered by means of the 3D-printed mold with effective dose coverage in PTV. The mold was accurately positioned at each treatment session by contact with the teeth. Furthermore, consistent placement provided dosimetric advantages. This patient received each fraction of the planned dose in full, as CT images showed no air gap between the 3D printed mold and palate surface. Indeed, a significant drawback with handmade molds is their impact on dose delivery as they may not adapt perfectly to the patient, particularly for superficial tumors, and may even need to be remade if gaps are found. Improper mold fitting may lead to an unwanted air gap between the mold and the surface… which could affect therapy…”
Creating Customized Oral Stents for Head and Neck Radiotherapy Using 3D Scanning and Printing
Introduction: Worldwide, head and neck cancer (HNC) accounts for more than 830,000 new cases per year with a mortality rate exceeding 430,000… and radiation therapy (RT) has demonstrated significant benefits in local tumor control and patient survival.
“However, RT is challenged by its inherent toxicity, notably radiation induced oral mucositis (RIOM),” which is a very common complication and “significantly detracts from patients’ quality of life, and may result in unplanned treatment breaks or a change in the therapeutic regimens. Therefore, therapeutic modalities and devices have been developed to tackle RIOM, and one of the most utilized devices is the oral radiation stent. They effectively displace and immobilize healthy tissue away from the radiation path, thereby improving the therapeutic index.”
The purpose of this study is “to evaluate and establish a digital workflow for the custom designing and 3D printing of mouth opening tongue-depressing (MOTD) stents for patients receiving radiotherapy for head and neck cancer.”
Materials and Methods: ”We retrospectively identified 3 patients who received radiation therapy (RT) for primary head and neck cancers with MOTD stents. We compared two methods for obtaining the digital impressions of patients’ teeth. The first method involved segmentation from computed tomography (CT) scans, as previously established by our group, and the second method used 3D scanning of the patients’ articulated stone models that were made during the conventional stent fabrication process.
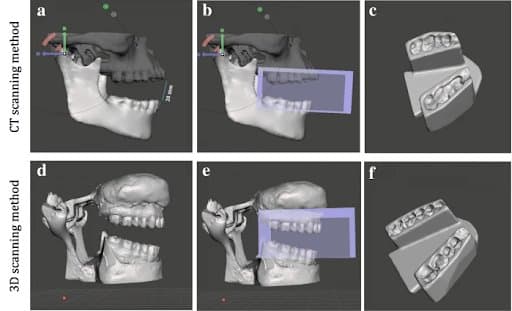
“Workflow for digital stent design using CT-derived STL files A&B&C), and the 3D-scanning method D&E&F). A&D) Mandibular rotation at Temporomandibular joint (TMJ) to achieve 20 mm inter-incisal opening; B&E) Acquiring negative impression of the teeth; C&F) Final completed stent” Three independent observers repeated the process to obtain digital impressions which provided data to design customized MOTD stents. For each method, we evaluated the time efficiency, dice similarity coefficient (DSC) for reproducibility, and the 3D printed stents’ accuracy. For the 3D scanning method, we evaluated the registration process using manual and automatic approaches.”
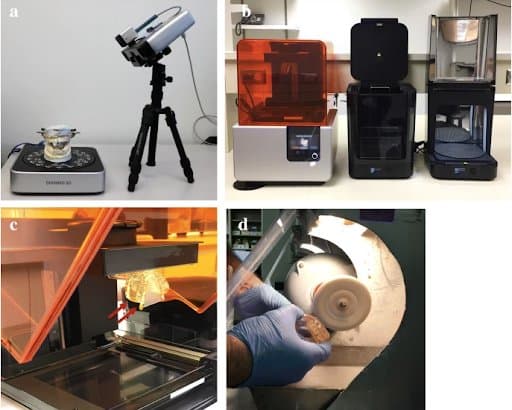
3D-printing process: A) Dental stone model placed on the rotating platform of EinScan-Pro desktop scanner B) FormLabs Form 2 printer, Form Wash and Form Cure unit assembly C) A 3D-printed stent attached (red arrows) to the build platform of Form 2 printer d Stent polishing using ground pumice stone and rag wheel apparatus.
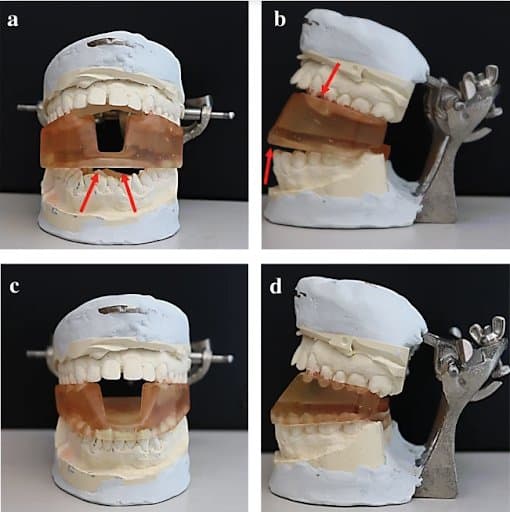
3D-printed stent positioned on the dental stone model of a patient with underbite. A&B) Frontal and lateral view of the stent made from CT scan segmentation. Arrows point to areas where the stent does not fit into the model. C&D) Frontal and lateral view of the stent made using 3D-scanning method.
“We used the Form 2 printer (FormLabs Inc., Somerville, MA) and Dental SG resin to print the stents. The 3D-printing process took approximately 4.5 h/stent and the layer thickness was 100 μm.”
Results: For all patients, the 3D scanning method demonstrated a significant advantage over the CT scanning method in terms of time efficiency with over 60% reduction in time consumed (p < 0.0001) and reproducibility with significantly higher DSC (p < 0.001). The printed stents were tested over the articulated dental stone models, and the trueness of fit and accuracy of dental anatomy was found to be significantly better for MOTD stents made using the 3D scanning method. The automated registration showed higher accuracy with errors < 0.001 mm compared to manual registration.
Discussion: “Radiation stents have been utilized for decades with variable degrees of customization. The conventional customized radiation stents are made by an oral-maxillofacial surgeon from patient's dental impressions… This conventional workflow is often challenged by the multiple appointments, intensive labor, time, and experience it dictates….
The combination of 3D-scanning, CAD, and 3D-printing showed a significant impact on the workflow and efficiency of the design and fabrication processes, which would help broaden their availability.”
Conclusion: “We developed an efficient workflow for custom designing and 3D-printing MOTD radiation stents. This workflow represents a considerable improvement over the CT-derived segmentation method. The application of this rapid and efficient digital workflow into radiation oncology practices can expand the use of these toxicity sparing devices to practices that do not currently have the support to make them.
A New 3D Printed Applicator With Radioactive Gel for Conformal Brachytherapy of Superficial Skin Tumors
Introduction: ”Basal cell carcinomas and squamous cell carcinomas are by far the most widespread cancers in the world…. Surface brachytherapy is an effective method in the treatment of skin cancer. Current skin brachytherapy techniques are based on the placement of a source of gamma or X-ray photons in a close distance from the skin to irradiate the lesion. Due to the nature of photons, radiation dose in these methods may affect healthy tissue as well as sensitive structures around the target. In order to minimize unwarranted and incidental exposure, we propose a new skin brachytherapy applicator based upon beta particles which have penetration ranges of a few millimeters in tissue.”
Materials and Methods: ”The proposed concept is radioactive gel housed within a pre-designed tumor-specific applicator matching the topology of the skin lesion….
A 3D printer (Formlabs, United States) was used to fabricate the physical model of the applicator with methacrylate photopolymers.”
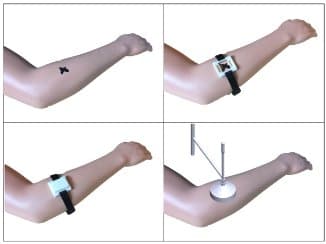
The workflow of the implementation of the treatment using the proposed surface brachytherapy applicator:
- Top left: skin tumor delineation including the safety margin
- Top right: fixing the applicator holder in the site of the tumor
- Bottom left: placement of the surface applicator for treatment delivery
- Bottom right: Brachytherapy of a skin tumor using a conventional surface applicator (for comparison)
Results: ”The particles mixed with the gel showed a uniform distribution pattern, which is an essential prerequisite in having a uniform dose profile on the skin surface. Based on the dose calculation data from the proposed concept, the dose delivered to the depth of 4500 μm in skin tissue is 10% of the dose delivered to the surface of the tumor, making it suitable for treating thin skin tumors especially when located on top of the bone.”
Discussion: ”The interesting feature of the applicator is that it is personalized. This means that the size of the applicator as well as the shape of its cavity (containment of radioactive source) are customizable to fit each specific tumor. Image of tumor, which is obtained by using imaging modalities, can be used to provide the basis for generating the digital model for the 3D printer. Manufacturing using a 3D printer provides an
opportunity for ease and quick preparation of this patient-specific surface applicator. Therefore, using this individually-fabricated applicator, radiation is shaped before entry the skin, sparing healthy tissue around the tumor surface.”
Conclusion: “We illustrated a new surface brachytherapy applicator for treating superficial skin tumors using a beta-emitting radioisotope. Combination of beta radiation therapy and 3D printing technology appears to well confine the radiation dose to the thin skin tumor while protecting the surrounding sensitive tissue.”
Prototype Testing the 3D-printed Montreal Split-ring Applicator (GYN) Using Biocompatible Materials
Introduction: ”The addition of interstitial needles to intracavitary GYN applicators (combined IC/IS) has been shown to improve the therapeutic ratio of locally advanced cervical cancer (stages IIIB-IVA) treatments involving tumor extensions to the parametrium. The multicenter EMBRACE II study protocol provides dose constraints as planning aims and dose limits for MR-delineated target structures. Commercial IC/IS brachytherapy applicators used to achieve EMBRACE II planning aims are expensive and only available in a few specialized centers, limiting the availability of this treatment option.”
Objective: “The purpose of this work is to show the feasibility of upgrading a widely used IC-only applicator; the CT/MR split-ring applicator (BEBIG Medical GmbH, Berlin, Germany) as the Montreal split-ring applicator which is suited for combined IC/IS brachytherapy. Adaptiiv Medical Technologies Inc. (Halifax, Canada) recently developed 3DBrachy, a software that allows users to create personalized 3D-printed brachytherapy applicators without knowledge of CAD software design. 3DBrachy’s Montreal split-ring software module allows users to create 3D-printable Adaptiiv caps with patient-specific needle trajectories that can be readapted between treatment fractions to improve conformity with the recommended planning aims. These caps are an improvement over a previously published non-printable generic template cap.”
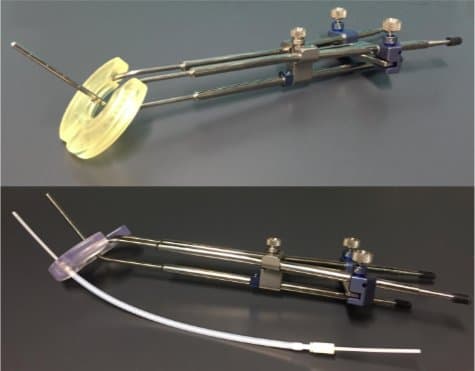
The Montreal split-ring applicator with IC/IS caps printed using Surgical Guide Resin (top figure) and BioMed Clear (bottom figure).
The bottom figure also shows attachment of a guiding tube used by the lunar ovoids of the Venezia IC/IS applicator with Proguide interstitial needles.
Methods: “CAD models of standard CT/MR split-ring 5 mm buildup caps were reproduced using Fusion 360TM. These caps were then made widder and integrated to 3DBrachy along with models of interstitial guiding tube notches. OncentraBrachy TPS (Elekta, Stockholm, Sweden) was used to produce a cap design preplans containing needle trajectories as reconstructed source paths that were exported as dicom RT-plan. In 3Dbrachy, the generic widened cap was co-registered and guiding tube notches were subtracted following the preplan needle trajectories to generate printable .STL files. Adaptiiv caps were then printed using a Form3 SLA printer (Formlabs Inc., Massachusetts, USA) using two resins; Surgical Guide (ISO 10993 biocompatibility & 50 μm resolution) and BioMed Clear (USP Class VI biocompatibility & 100 μm resolution) as shown in figure.”
Results and Discussion: “As shown [in the figure below], Adaptiiv caps prototypes were printed and tested for the following properties both pre- and post-sterilization:
1. Smooth gliding of the titanium split-ring into the printed canal.
2. Secure attachment of interstitial guiding tube notches.
3. Proper fixation using the original CT/MR attachment screw.”

The left figure shows a CAD example of a cap pair with interstitial needles that can be produced using 3DBrachy’s workflow. The right figure shows post-sterilization fixation of the attachment screw with a cap printed using Surgical Guide Resin for prototype testing.
“The printed prototypes were verified to be functional following the successful testing of the properties stated above. In particular, secure attachment of guiding tube notches for interstitial needle obliquity angles of 15°, 30° and 45° was verified. Fixation screw thread was found to be the most sensitive feature of the printed caps. A minimum resolution of 0.1 mm in 3DBrachy was found to be necessary for proper screw fixation using BioMed Clear printed with a layer height of 100 μm. Using these settings, the number of times the screw could be re-used before stripping the threads was found to exceed 10 times which is satisfactory considering the disposable nature of these caps. The sterilization protocol involved steam sterilization at 132 °C in an autoclave for 4 minutes followed by a 25 minutes dry phase which was not found to negatively impact the results for prototype testing.”
Conclusion: “Stereolithography-based 3D-printing technology was successfully used to produce prototypes of the Montreal split-ring applicator suited for combined IC/IS brachytherapy. A dedicated module in Adaptiiv’s 3DBrachy software allows users to design Adaptiiv caps with patient-specific needle trajectories. Prototypes printed with Surgical Guide and BioMed Clear resins were verified to be functional both pre- and post-sterilization for interstitial needle obliquity angles ≤ 45°. Future studies will aim to characterize dosimetric advantages of using Adaptiiv caps with patient-specific needle trajectories over generic needle trajectories used by commercial IC/IS applicators.”