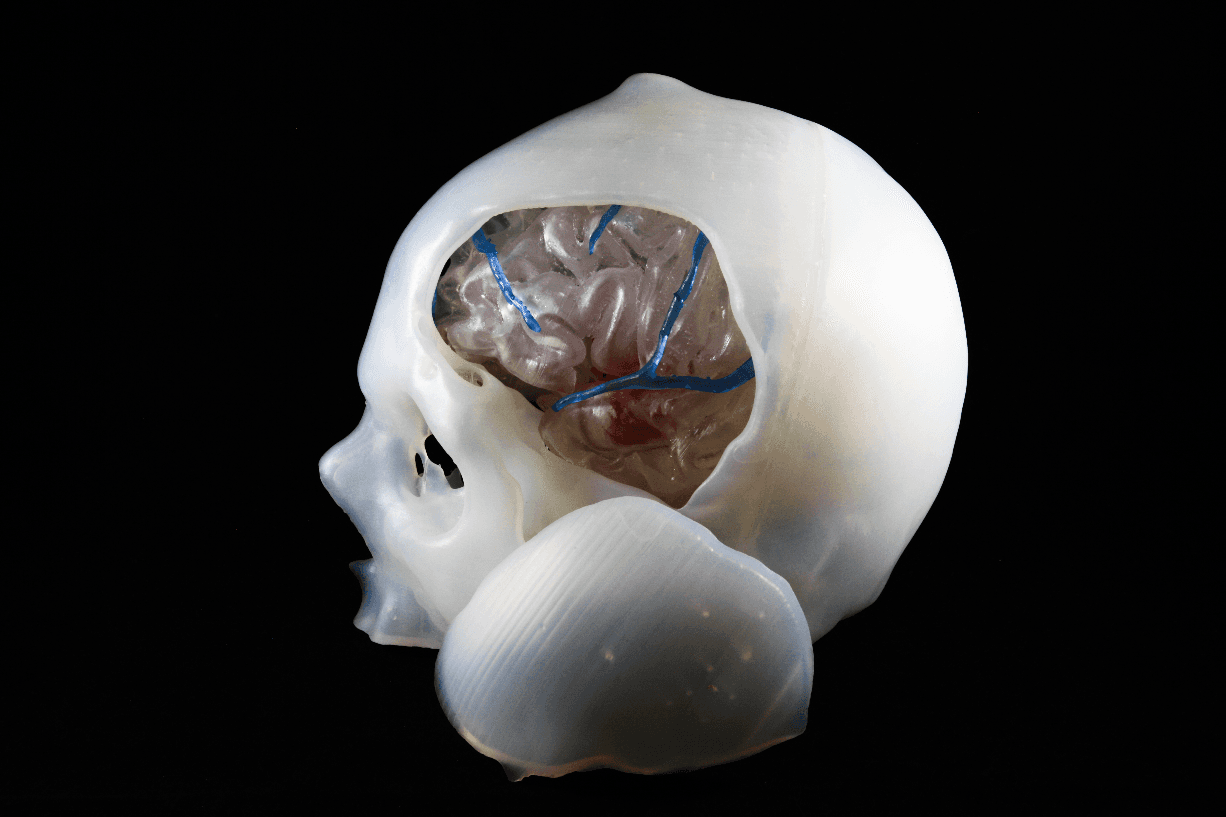
3D printed skull, with exposed brain and arteries, used for practice craniotomy, generated by Trabtech Team (https://trabtech.co)
In recent years, advances in intravascular technology have helped reduce the need for surgeries to address brain aneurysms. Minimally invasive intravascular techniques are now used in the majority of low-complexity brain aneurysms. For more complex and severe cases, where intracranial surgery is absolutely necessary, 3D printing has been adopted as an intraoperative guidance and planning tool to lower risk and improve outcomes. One of the leading surgeons in this area, Sahin Hanalioglu, MD, of Hacettepe University Department of Neurosurgery, has been a pioneer in using 3D printed models to improve surgical outcomes. He was also assisted by Prof. Dr. İlkan Tatar from the Anatomy Department of Hacettepe University. Trabtech Medical Advanced Technologies’ R&D and application team, who has deep expertise in 3D anatomical modelling, planning, and more importantly 3D printing, have been intgerated into the 3D anatomical modelling and printing processes (in coorperation with surgeons) of many patients with a sizable brain aneurysms.
Problem: In the case below, a patient has a sizable brain aneurysm. An aneurysm is a vascular malformation (a bulge in a blood vessel caused by a weakness in the blood vessel wall), and if an aneurysm of the brain vessels ruptures, it can cause a brain hemorrhage. Additionally, if an aneurysm gets thrombosed (when blood clots block veins or arteries), it can be a source of embolism.
Solution: Exclude this aneurysm from normal brain circulation. The aneurysms normally are buried deep within the brain and in order to reach them, microsurgical techniques are required to carefully split the brain fissures and natural corridors carefully, dissecting circumferentially. Eventually, the aneurysm will be excluded from circulation by surgical clips and the wound will be closed. This procedure is called clipping.
Conventional Method Compared to 3D Printing: Traditionally brain surgeons use CT or MRI images, along with their own anatomical knowledge, to imagine the three-dimensional relationship of the pathology in their mind. Now, with 3D printed technology and 3D simulation, they can easily see the tangible anatomy both on the screen (3D VR headset) and also on a 3D printed model.
The 3D visual simulation technology has made incredible advances in recent years, but for many surgeons, physical touch and practice on a customized model can have an even greater positive impact on surgical outcomes. The multi-layer, segmented, and fully integrated models by TrabTech can help with craniotomies, where surgeons must drill into the skull and remove a portion to create a ‘surgical window,’ without damaging the tissue beneath.
This unique model not only allows surgeons to visualize but also helps them to simulate the surgery. Surgeons have the opportunity of rehearsing the surgery and apply different approaches to attack the pathology before the actual date to understand the advantages and drawbacks of certain surgical techniques and also explore the obstacles.
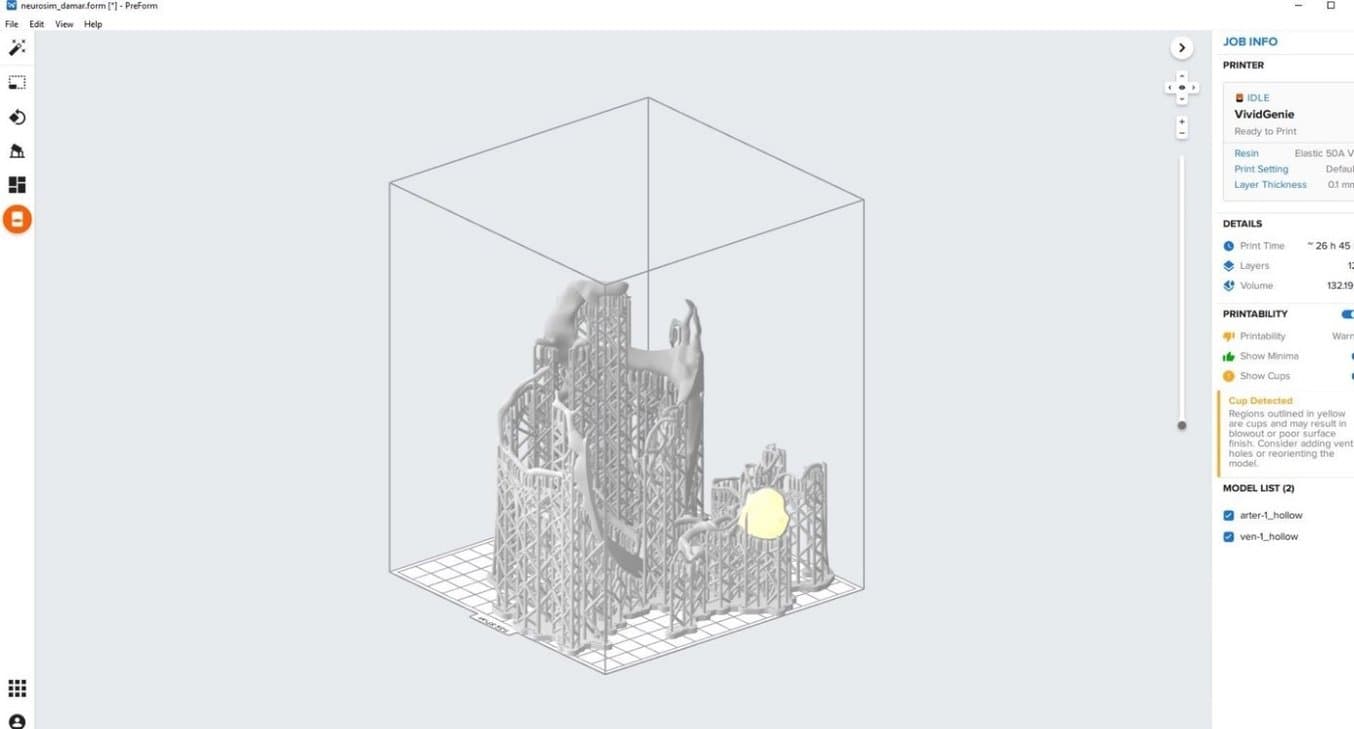
The team used PreForm print preparation software to orient and print the parts.
Importantly, using 3D printed models can help bolster confidence before a complex procedure. “You are not going to see any surprises during the surgery, you can rehearse everything before the operation. That is instrumental in my own practice and to many surgeons that I talk to,” said Hanalioglu.
Other Benefits of 3D printing: 3D printed models are also important for educating postgraduate and graduate students as well as patients. There are different radiological modalities like MRI angiography, and three-dimensional volumetric tomography MR venography to have fully sophisticated models. However, each modality can visualize one or two specific inner structure tissues of the brain like diencephalic structures or ventricular structures. But the brain structures anatomically change or get shifted when there is additional pathology like a tumor. “Therefore we need to re-visualize and reconstruct the new shape of the normal tissue depending on the type of pathology. These models are customized and fully personalized models, depending on the patient's diseases or pathologies,” said Hanalioglu.
Hanalioglu told us that, “sometimes, in a complex surgery, only the head surgeon may be fully aware of where the problems are in the patient. Now, with the 3D printed models, everyone, even the residents, go into the operation with knowledge. It facilitates your intraoperative guidance.”
He continued, saying that, “these 3D printing models will help us to rehearse the surgery with residents, students, and other colleagues. When you have the 3D printed model it becomes valuable for training medical students and residents or young neurosurgeons to discuss surgery,” said Hanalioglu.
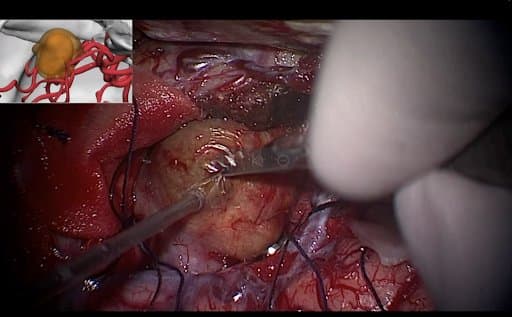
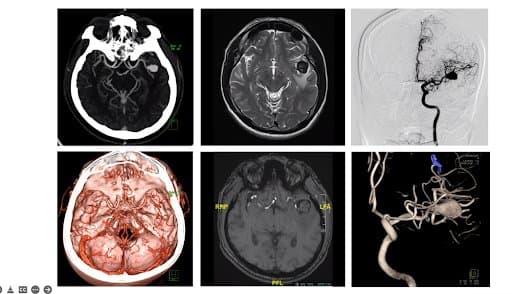
Here, on the right, different modalities show the different parts of one single reality which is this three-dimensional pathology. But once you have the 3D printed model, you have all those different pieces of information together in one piece. On the left, an operation in progress.
How to create 3D models: TrabTech used Materialise software (Mimics) for model segmentation. A biomedical engineer uses this software to import each DICOM file taken through different modalities. The segmentation, modeling, and simulation process will be done by the software features and the final file will be exported in .stl or .obj format. The surgeon can also be involved in this process to help define the pathology, and fine-tune the final digital file to be printed. For example, the surgeon could help identify an interference between two vessels, using their expertise to double-check each model. Despite the high resolution of imaging techniques, a second opinion is invaluable for such complex systems.
Patient Perspective: A 55 years old patient presenting suspicious seizures was analyzed and evaluated first with brain imaging via CT and MRI scans. The brain imaging revealed a 1.5 cm mass in the left Sylvian fissure between the frontal and temporal lobes of the brain. The first assumption was a huge tumor or a possibility of an aneurysm. After further imaging, it was confirmed that the case was a thrombosed giant aneurysm (greater than 2 cm). When a thrombus is found within an aneurysm, the small and thick thrombi (blood clots) can wander to distal arteries, blocking them. Those blockages will stop blood flow to important parts of the brain, causing strokes in the patient.
At the time surgical treatment was presented as an option, the medical team had used the digital models of advanced imaging techniques like CT, MR, MR angiography, and 3D rotational digital subtraction angiography, and discussed surgical planning with the patient. For an acute situation like this, requiring urgent surgery, using a 3D model can help the surgeon envision and practice as well as help the patient become comfortable with the idea of the procedure.
As can be seen in the digital simulation, the color, the angles, and the positions of the digital model can be changed, and the final surgery can be simulated. This image shows the complex relationship of the center prisms with the underlying vessels. The model allows surgeons to see the relationship of the main branches beneath the brain and the simulated clipping before the surgery, so when they prepare for the surgery the visual information is readily accessible, leading to more efficient procedures.
Challenges and Considerations: One downside to using 3D printing is the turnaround time it takes to create the parts. Hanalioglu told us that he needs more than just one or two days to fully prep and print his models. So for urgent cases, it might not be possible to create 3D models.
Surgeons also have to make sure they have the right equipment, which includes a high-resolution scanner and quality 3D printer.
According to Hanalioglu, when considering a 3D printer, the top traits he considers are:
- The ability to print both hard and soft materials. This is because his models contain both the skull and arteries.
- Part resolution is important, to help simulate the operation as closely as possible.
- Costs need to be reasonable on a per-part basis.
3D Printing, Cadavers, and Surgical Planning: Most practitioners accept 3D printed models as a complementary tool, not a replacement for cadavers. However, there are limitations to a purely cadaver-based study practice, and institutions are using 3D printed models more and more to help close any knowledge gaps at low cost.
If the residency group is crowded with lots of students, the professors cannot teach each student individually with cadavers. “Cadavers can be used for basic instruction, then more detailed process rehearsals can be done with 3D printed physical models. Of course, depending on the level of medical students, the 3D printed model’s details can be adjusted. For example, coloring various parts of the model can be helpful for newer students,” said Hanalioglu.
Therefore, both 3D printed models and cadavers should be used in concert to provide maximum value in medical education.
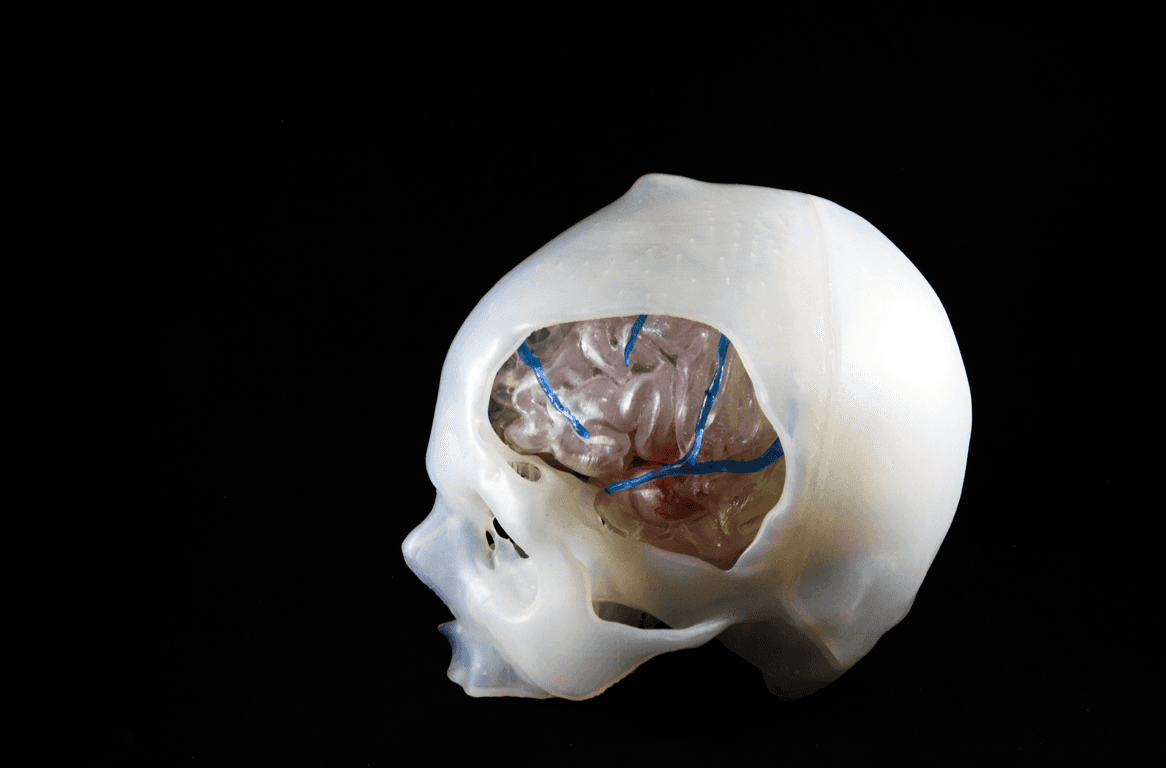
3D printed skull, with exposed brain and arteries, used for practice craniotomy.
The nice part of a 3D printed model is that the brain is transparent and the aneurysm and vessels beneath the temporal and frontal lobe of the brain can be easily seen. The importance of the physical 3D printed model in comparison with 3D digital models can be clearly seen when the surgeons are not experienced enough to handle the surgery! The 3D printed model can help inexperienced surgeons to standardize the aneurysm position and craniotomy.
Although the 3D digital models allow you to adjust and segment virtually like changing the position, there is a lack of haptic feedback. In a 3D printed model, surgeons can have different angles of the brain by changing their own positions. It is, however, not reversible once the model is damaged or cut.
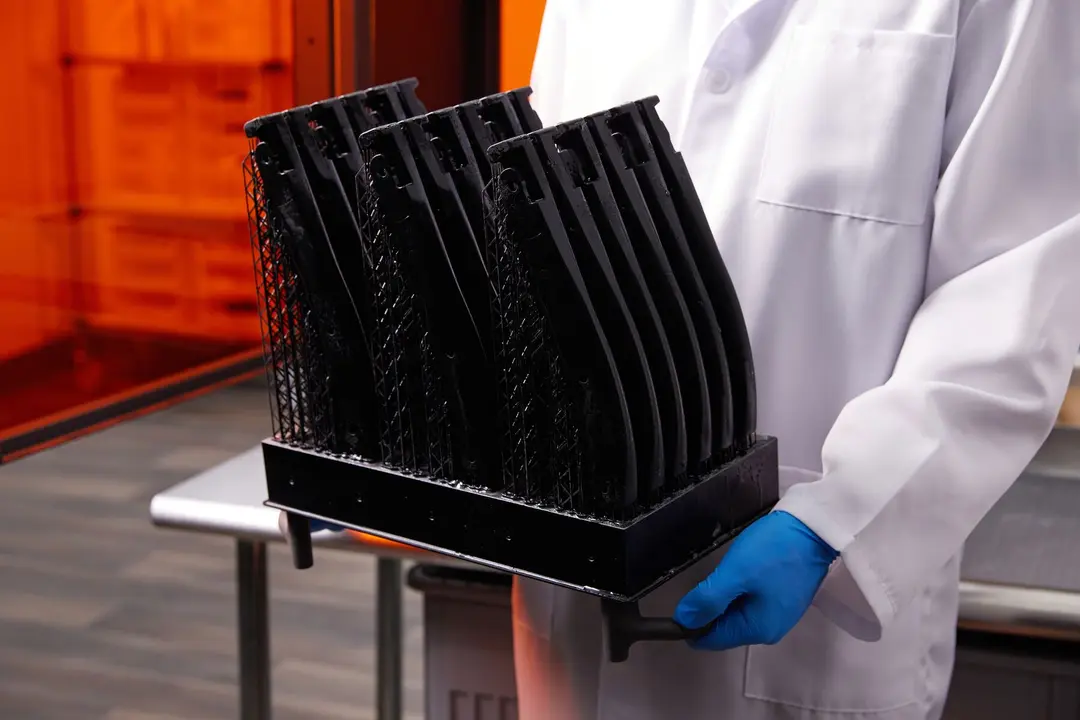
Materials used for 3D printed models: In this 3D printed model, the brain vessels, tissue, and skull anatomy have been acquired by imaging, with Durable Resin being used to print bone models, and Elastic 50A Resin being used to print brain tissues and vessels. Models were printed on the Form 3, which has recently been replaced with the new Form 3B+.

Hanalioglu has used Elastic 50A for its elastomeric properties; its ability to mimic artery tissue is helpful for accurate practice. According to him, in recent years, “there have been improvements to the materials. They feel a lot more like arteries. There is still room for improvement, but they feel better.”
Finally, Hanalioglu has his printed artery models painted to help assist with identification of various parts. The ability to paint a soft material like Elastic 50A Resin is another benefit of the material.