As more instruction moves to the virtual classroom and the cost of patient-specific, 3D printed simulation models from CT/MR data has decreased to a few dollars per part, a rapidly increasing number of residency programs are creating detailed, patient-specific models to enhance trainee education both at home and in the classroom. In-house 3D printing is helping programs achieve their goal of training the next generation of surgeons with proven, next generation technology.
In this post, we explore how 3D printing is being used to improve surgical resident education.

The Training of Resident Physicians
The education of physicians has historically been an apprenticeship. Once the curriculum of lectures and classroom-based education was complete, the student would enter residency. The term ‘resident’ gives the average person an idea of what is required. Often, physicians would be so consumed with caring for sick patients that they essentially lived within the hospital. This traditional method of medical apprenticeship often required trainees to devote almost 100 hours per week for three to seven years to medical education, often at the expense of self-care and the ability to have a life outside of medicine. This all changed in 1984, in the highly-publicized case of two overworked medical residents who made an error that resulted in the accidental death of a college student. This eventually led to restrictions on the total number of hours per week residents could work, known as resident duty hours.
Resident Duty Hour Restrictions – Doing More with Less
While the purpose of resident duty hour restrictions is exemplary, to reduce physician fatigue and ensure adequate rest between shifts, these restrictions have led to a significant decrease in the total time that medical and surgical residents spend in the hospital learning how to operate and take care of patients. With this reduction in the overall volume of training, residency programs have been forced to adopt more efficient methods of educating the future surgeons of America. Today, residents simply do not have any time to waste, the hours they spend in the hospital need to be efficient, because they don’t have the same amount of time to become proficient surgeons as their predecessors did.
3D Printing to Improve Surgical Resident Education
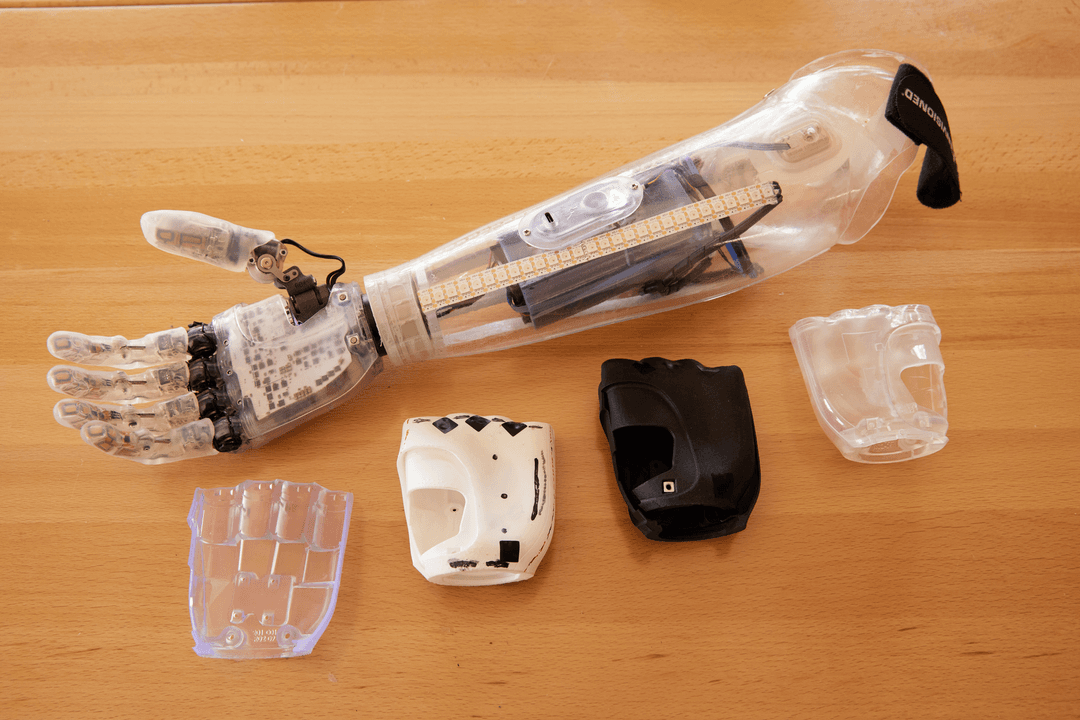
In order to help improve resident’s overall education, surgical residency programs across the country have searched for solutions. Some programs have added more lectures and others have added in virtual reality simulations, many programs have opted to increase their use of hands-on tools to improve their residents’ education. Surgery is inherently a ‘hands-on’ specialty, surgeons diagnose a problem in their patients based on symptoms or imaging findings, and then take the patient to the operating room to address the problem. Because of this ‘hands-on’ connection, 3D printing has been applied by several surgical residency programs in order to improve the education of their surgical residents.

Patient Specific 3D Printed Models for Surgical Resident Education
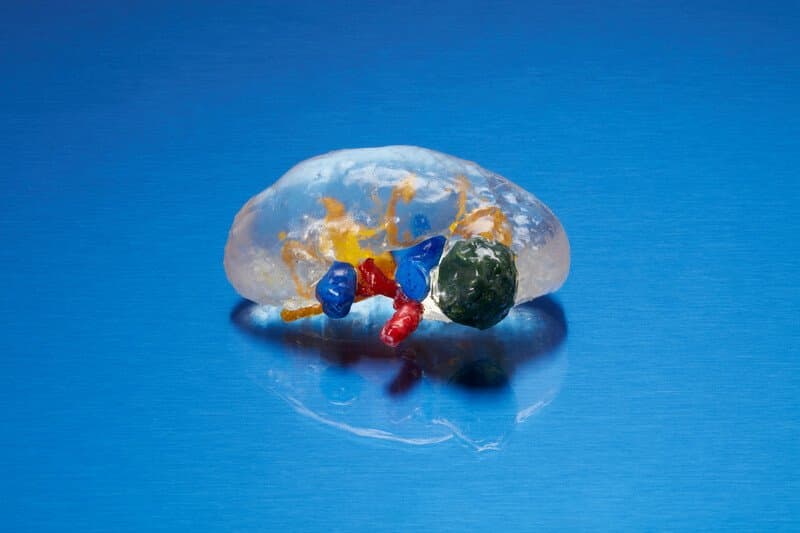
As one would expect, brain surgery can be a complicated endeavor. Surgery of the skull base can be even more complex, because many of the most important structures in the head such as the blood vessels that give life to the brain and delicate nerves are situated there. When tumors occur in this region, they can envelop the blood vessels and nerves or distort the normal anatomy. Neurosurgeons at several institutions, including Stanford, the University of Pittsburgh, and Johns Hopkins, have sought to improve the safety of skull base operations by utilizing 3D printing1. A recent research study published by this group reported on their experience using 3D printing to plan for four different operations and noted that the cost per operation ranged from $3-41 for the raw materials. The authors concluded that based on their experiences, the 3D printed patient-specific models were helpful not only for surgical planning but also for intraoperative use, in order to better understand the anatomy as the tumor is being resected. They also noted that “Patient-specific 3D printed models may be used to enhance understanding of particular approaches and relevant anatomical landmarks encountered”1.
In addition to neurosurgical resections, physicians have also encountered success in using 3D printing to help illustrate concepts when they’re teaching medical students. The addition of 3D printed teaching tools can begin as early as medical school, where there is clear evidence that students learn well from supplemental teaching aids. For example, cleft lip or palate is a congenital abnormality that can be difficult for medical students to visualize. One group of researchers tested how effective 3D printed models were in medical student education by teaching one cohort with the models and one without, and then giving both the same test to assess how much the groups had learned2. The doctors found that for the 67 students included in the study, the addition of 3D printed models to the lecture raised test scores by over 30% (p = 0.038).
3D Printing for Resident Simulation + Preoperative Planning
Perhaps the most exciting use of 3D printing in medical education is the creation of simulators or patient-specific models for rehearsing an operation prior to actually performing it on a patient. Research conducted by the neurosurgery department at Vanderbilt University showed that utilizing 3D printed spine models, their residents were able to train on a simulator and improve their placement of spinal instrumentation by over 60%3. The authors first had the residents practice placing the instrumentation, then administered a brief instructional review of appropriate placement techniques and then had the residents attempt the same task again. The authors noted that the 3D printed simulators were cost-effective, the associated materials to print each simulator cost between $5-12.
One group of endovascular surgeons in Brazil assessed the impact of practicing endovascular aortic aneurysm repair on a 3D printed, patient-specific simulator prior to performing the real procedure4. They created two groups, one which utilized the 3D printed simulators and one group who simply performed the procedure as normal. The group that practiced reported that not only did the practice subjectively increase their confidence going into the surgery, but utilizing the 3D printed models to practice was associated with a nearly 30% reduction in the total procedural time and the amount of X-ray radiation used, as well as a reduction in the contrast dye used. This real-world application of 3D printing in surgical education demonstrated not only subjective improvements in trainee confidence, but real, objective improvements in outcomes related to patient safety such as X-ray and contrast dye usage and total procedural time.

Closing & References
The training of competent, technically gifted surgeons is of the utmost importance to ensure that quality medical care continues to be delivered in the United States and across the world. In the past, physicians and surgeons acquired their skills partly by being in the hospital around the clock. As ever-present learners, they were able to learn from their mentors how to safely operate and treat their patients.
Today, the educational paradigm has shifted, and resident work hour restrictions limit the total amount of time that can be spent in the hospital learning. With this reduction in total time spent in direct patient care, other methods of learning which utilize 3D printing, such as surgical simulators or the generation of patient-specific models, are being explored by surgical residencies with the goal of supplementing the resident’s hands-on training. The initial application of these methods has been met with enthusiasm and has demonstrated meaningful, measurable impact of resident learning. As virtual classrooms become the new norm, low-cost simulation models can also support student and trainee education within their own homes.
References
- Panesar SS, Magnetta M, Mukherjee D, et al. Patient-specific 3-dimensionally printed models for neurosurgical planning and education. Neurosurg Focus. 2019;47(6):E12.
- AlAli AB, Griffin MF, Calonge WM, Butler PE. Evaluating the Use of Cleft Lip and Palate 3D-Printed Models as a Teaching Aid. J Surg Educ. 2018;75(1):200-208.
- Bow H, Zuckerman SL, Griffith B, et al. A 3D-Printed Simulator and Teaching Module for Placing S2-Alar-Iliac Screws. Oper Neurosurg. 2019;18(3):339-346.
- Torres IO, De Luccia N. A simulator for training in endovascular aneurysm repair: The use of three dimensional printers. Eur J Vasc Endovasc Surg. 2017;54(2):247-253.