On Shirley Anderson’s left shoulder is a faded heart tattoo that says “Della,” his wife of fifty years. They met as high school sweethearts in Evansville, Indiana and married right before Shirley served in the navy in the Vietnam war. When he returned, he worked as a mechanic, and she was an administrative assistant. They soon had two children and later, three grandchildren. They still live in Evansville and have enjoyed a remarkably happy marriage through the years. To this day, Shirley carries around a picture of Della in his wallet.

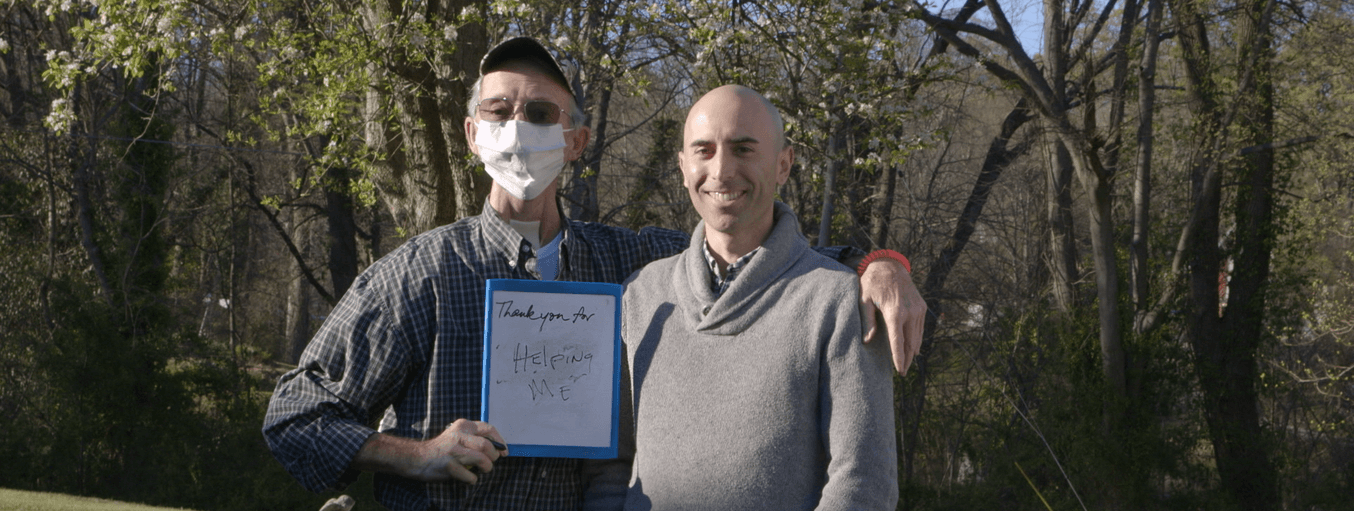
Their strong marriage was shaken in 1998, when Shirley discovered a cancerous lump on his tongue. From that point on, Della says, “It’s kind of been one bad thing after another.” For years, Shirley endured surgeries and radiation therapies. Doctors put a radium implant in his jaw, which destroyed his facial tissue. Surgeons removed his chest muscles to recreate his lower face, but it didn’t work — in the end, he was left without a jaw and Adam’s apple. Because he couldn’t eat solid food, he lost 80 pounds in three months. He now wears a surgical mask in public to hide his lower face. He usually speaks by writing on a handheld whiteboard or by communicating through Della.
Their luck began to change in 2012 when they met Dr. Travis Bellicchi, a resident at the Indiana University School of Dentistry who specializes in maxillofacial prosthetics. Shirley’s case was a huge challenge — he required a facial prosthesis that was about four times larger than anything made at IU. Yet Dr. Bellicchi was determined to create an artificial jaw for Shirley.

At first, Dr. Bellicchi used traditional techniques to make Shirley’s prosthesis. With this method, Shirley had to sit with plaster on his face for several hours. Some patients who undergo this procedure panic because of the claustrophobic feeling of their face covered in plaster, requiring them to breathe through a straw. Next, Dr. Bellicchi cast a replica of Shirley’s face in gypsum that was used to sculpt the prosthesis in clay. He used that sculpture to cast the final silicone version. An artist painstakingly handpainted the surface to match Shirley’s skin tone, a process called aesthetic characterization. Despite its many shortcomings, this has long been the standard method for creating artificial facial parts.
“The traditional process for impression, sculpting, moldmaking, and aesthetic characterization is a laborious task,” Dr. Bellicchi explains. The prosthesis was so uncomfortable that Shirley couldn’t wear it for more than four hours at a time, it was so heavy that it often slipped down, and the surface lacked realistic skin details. Dr. Bellicchi says, “I knew there was a need for a digital solution.”
Professor Zeb Wood, a lecturer at the School of Media Arts and Sciences, connected Dr. Bellicchi to digital scanning, digital sculpting, digital moldmaking, and high-resolution 3D printing. For Shirley’s new prosthesis, instead of the uncomfortable impression process, they created what they call a “virtual patient” — a digital model of Shirley’s face using CT scan data to capture bone detail, overlaid with a 3D facial scan. Dr. Bellicchi watched in amazement as Cade Jacobs, an IU student, designed a prosthesis in ZBrush 3D sculpting software in a fraction of the time it would have taken to sculpt it in clay.
“They really couldn’t believe how easy it was. They had been struggling to get the same results for a long time when they were using the traditional process.” — Cade Jacobs

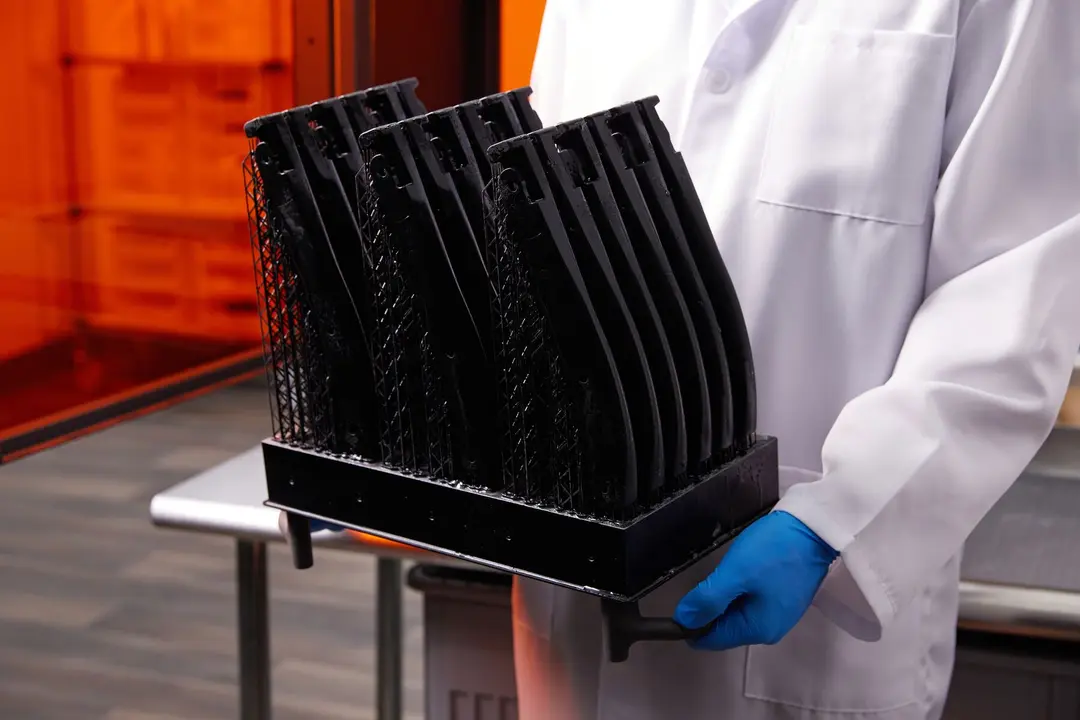
The team used Formlabs 3D printers to turn the digital sculpt into a 3D printed mold, ready to cast for the final prosthesis. They had originally experimented with FDM printing, but they preferred the Form 2 SLA 3D printer because it captures intricate, pore-level surface details and provides a watertight mold.
The new 3D printed mold has a number of improvements on the original. It looks more realistic and is much lighter and more breathable so that Shirley feels comfortable wearing it for a longer period of time. The new prosthesis also has a “feather-edge margin” around the outside, a tapered silicone edge that creates a more natural break.
“We’ve used 3D printing to replace about 75 to 80% of the process in traditional prosthetic fabrication.” — Dr. Travis Bellicchi
“We started with Shirley Anderson,” Dr. Bellicchi explains. “And we’ve expanded that worfklow to several other patients.” One patient is Jackie Barnard, a man who lost his left ear in a traumatic accident. On their very first meeting, Dr. Bellicchi took a digital scan of Jackie’s face, and Cade got to work at making a digital sculpt. On Jackie’s second visit to IU, just six weeks later, Jackie and his family were presented with a prototype of his new left ear and the surgical guide they would use to align the prosthesis for attachment.

The IU team has applied this groundbreaking method to six other patients and continue to seek candidates. Dr. Bellicchi is thankful that Shirley was the first patient. He says, “It’s a privilege to have an opportunity to work with a patient like Shirley because Shirley makes the process collaborative. Shirley participates in my work to improve his prosthesis. Although it’s likely the most significant challenge I will ever face in my prosthetic career, I think it may be the most rewarding.”
Today, Shirley and Della Anderson focus not on what they’ve lost but on what they still have. Shirley recently wrote on his whiteboard, “I have my life going just as I want.” Now, he has something that very few people have — a medical process named after him. Dr. Bellicchi calls the new digital method of creating artificial facial parts “The Shirley Technique.”
Have a question about the Shirley Technique? Get in touch with the IU team at [email protected].
The Future of Healthcare is Now
Learn more about how healthcare providers across the globe are using professional-grade desktop 3D printing for high-impact medical applications, while saving organizations significant time and costs from the lab to the operating room.
Interested in 3D printing patient-specific models? Download our white paper for a step-by-step walkthrough of the workflow for creating high-accuracy tactile reference models for preoperative planning, enhanced patient consent, intraoperative visualization, and sizing or pre-fitting medical equipment.