A 3D printed bolus devices printed with BioMed Clear Resin and BioMed Amber Resin.
Cancer is a leading cause of death around the world. Over time, medical professionals have increasingly turned to radiation therapy as a powerful tool for fighting cancer and saving patients’ lives. However, radiation is toxic and dangerous if not correctly administered. In order to provide a targeted dosage to the affected superficial layers of the skin, bolus materials are employed to help medical professionals precisely control radiation dosing of the cancerous tissue while limiting unwanted radiation exposure to healthy tissue.
As 3D printing has seen a rapid rise in adoption in hospital settings, it’s worth asking the question whether it is possible to 3D print a skin-safe, patient-specific bolus which conforms to the patient's unique anatomy.
The answer is a resounding yes. 3D printed bolus are not only safe and accurate --- they are in fact already being manufactured and deployed in hospitals around the world.
Recently, Formlabs hosted Greg Gagnon, the 3D printing specialist at Baystate Health, and Senior Product Manager at Adaptiiv Medical Technologies Inc, Borko Basaric, to review the current state of 3D printing bolus devices.
3D Printed Bolus Devices: Challenges & Solutions
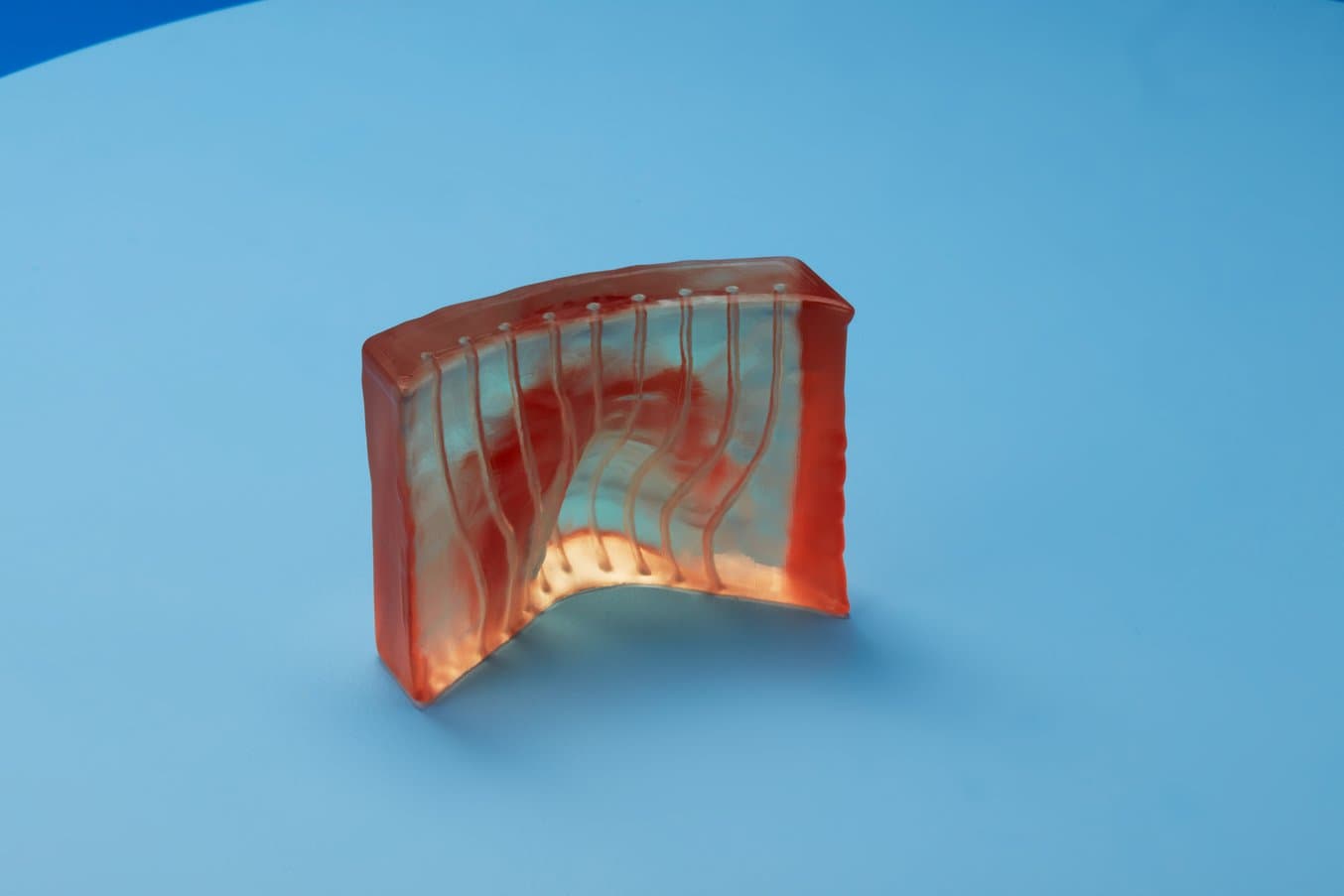
3D print bolus with visible channels. BioMed Amber Resin's transparency allows for improved device accuracy with superior dose distribution.
Traditional treatments come with a host of problems for medical professionals. This can degrade the patient experience, and result in reduced performance of the radiation treatment.
Some of the problems with the way bolus devices are created now are:
- Complex patient setup can take many hours.
- Inability to accommodate or correct for anatomical irregularities.
- Air gaps between accessory and skin can cause underdose.
- Manual fabrication can be laborious and yield unpredictable results.
- Bolus must be shaped and secured in place each visit.
- Skill shortage of staff that can create accessories.
- Materials, such as Freiburg flap, can be expensive.
Traditional bolus setups for patients can be crude, take multiple days to create, and include hot wax and mesh face coverings. They also require continuous checks to make sure the radiation tubes are properly aligned. Furthermore, the traditional process requires highly skilled staff trained in working with bolus devices. This point has been exacerbated by recent hiring shortages in the United States, putting pressure on hospitals to find new methods to apply radiation therapy.
The solution to these problems is in-house production of bolus devices using 3D printing. “Our mission is to have an applicator that perfectly fits the patient,” said Basaric. While this has always been a goal of medical professionals, it simply wasn’t viable before the advent of in-house 3D printers.
- By using 3D printers to create bolus devices, hospitals benefit from:
- Patient-specific devices and the elimination of manual creation of devices.
- Improved device accuracy with superior dose distribution.
- Variable trajectory settings
- Wider pool of staff able to produce devices
- Less time required for design, fabrication, and set-up.
- Cost reductions due to significant cost savings.
Baystate Health, the largest hospital system in Western Massachusetts, has seen great success switching to 3D printed bolus devices. Gagnon told us that, “since our hospital set up a shared portal for me to get the patient file, I can turn the part around in 24 hours. I normally request extra time, but the prints sometimes only take eight hours. I can sit at my home office and send the file to my printer in the office, and when I come into the office, it’s done.”
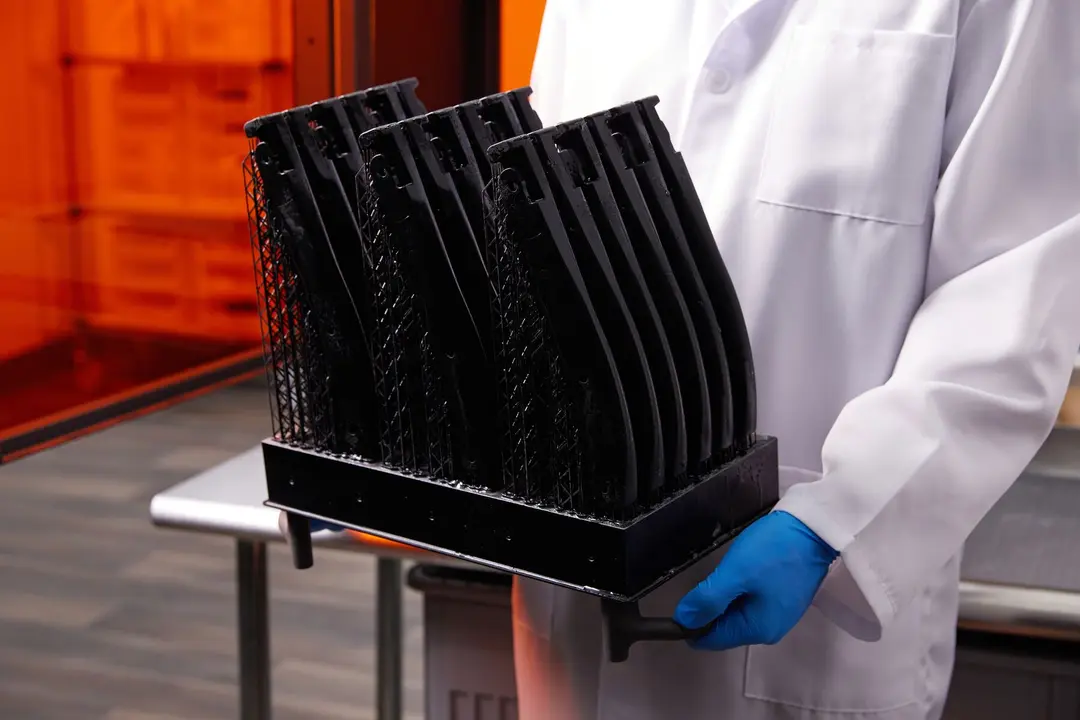
The ease of use was notable, with Gagnon saying. “The printing process is easy, we print the bolus device right on the build platform. The 3D printing resolution is so good that you don’t need supports inside the channels.”
While this workflow can be used with FDM 3D printers, SLA will provide a more consistent print throughout the device, never leaving gaps and air pockets in the print. Gagnon often turns to Clear Resin to make his devices. Clear Resin polishes to near optical transparency, making it ideal for showcasing internal features where the tubes need to be placed.
FDM & SLA 3D Printing For Brachytherapy
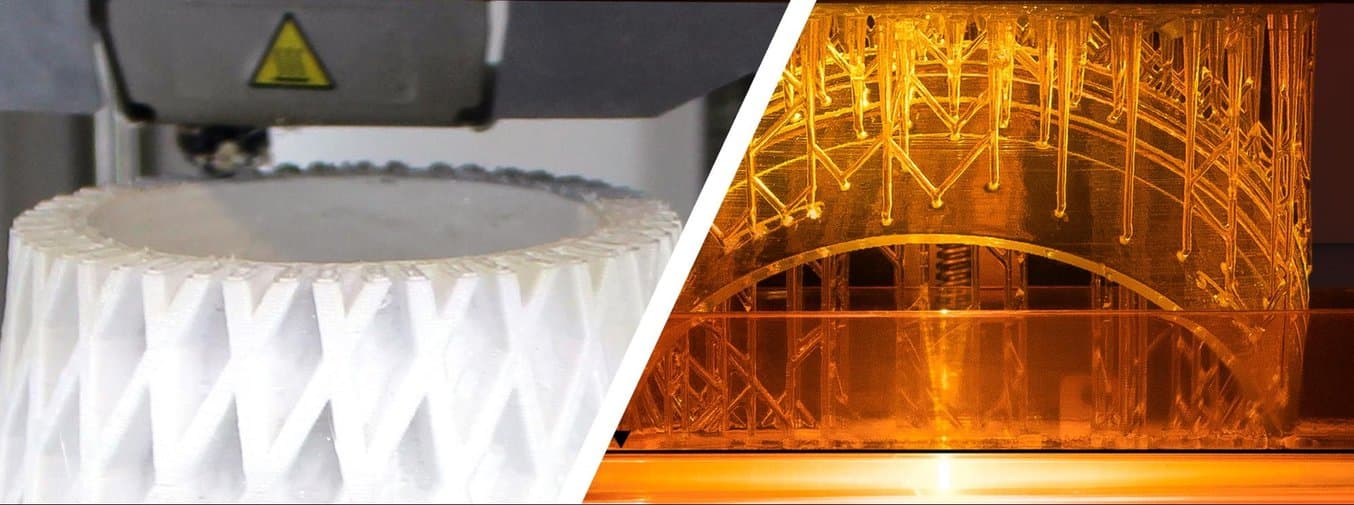
Bolus devices can be printed using either FDM or SLA 3D printers. What is the difference?
- Fused deposition modeling (FDM), also known as fused filament fabrication (FFF), is the most widely used type of 3D printing at the consumer level. FDM 3D printers work by extruding thermoplastic filaments, such as ABS (Acrylonitrile Butadiene Styrene), PLA (Polylactic Acid), through a heated nozzle, melting the material and applying the plastic layer by layer to a build platform. Each layer is laid down one at a time until the part is complete.
- Stereolithography (SLA) 3D printers use a laser to cure liquid resin into hardened plastic in a process called photopolymerization. SLA resin 3D printers have become vastly popular for their ability to produce high-accuracy, isotropic, and watertight prototypes and parts in a range of advanced materials with fine features and smooth surface finish. SLA resin formulations offer a wide range of optical, mechanical, and thermal properties to match those of standard, engineering, and industrial thermoplastics.
Learn More: Brachytherapy Case Study
You can gain access to the full video featuring Greg Gagnon, the 3D printing specialist at Baystate Health, and Senior Product Manager at Adaptiiv Medical Technologies Inc, Borko Basaric, at the link below (part of the User Summit 2022 event archive). Here you can see a full case study done with an 80 year old male patient with bilateral BCC of shins. Gagnon also gives advice to hospital staff looking to justify investments in 3D printing, and talks about his workflow for creating bolus devices.