High Tibial Osteotomy
Clinical Experience Using a 3D-Printed Patient-Specific Instrument for Medial Opening Wedge High Tibial Osteotomy
Introduction: “High tibial osteotomy (HTO) has been adopted as an effective surgery for medial degeneration of the osteoarthritis (OA) knee. However, satisfactory outcomes necessitate the precise creation and distraction of osteotomized wedges and the use of intraoperative X-ray images to continually monitor the wedge-related manipulation. Thus [traditional] HTO is highly technique-demanding and has a high radiation exposure. We report a patient-specific instrument (PSI) guide for the precise creation and distraction of HTO wedge.”
“The PSI rationale is to create a guiding instrument for the surfaces that can fit well with the targeting region of the patient's bone. The benefits include increased accuracy, decreased surgery time, and elimination of the need for extra devices or reference markers.”
Methods and Materials: “Ten patients (4 males and 6 females) voluntarily enrolled in this study… All patients were diagnosed as medial OA knee with varus deformity… Preoperative X-ray and computed tomography- (CT-) scanning images were used to design and fabricate PSI guides for clinical use… The correction angle was determined by preoperative weight-bearing coronal plane radiography of the entire leg”

Intraoperative photograph with the PSI guide
“A surgical guide was designed to fit the medial tibial surface with four pin holes to stably fix the guide on the targeting region of the patient's bone. A cutting slot and a guiding plane were provided for the biplanar osteotomy… For intraoperative confirmation of the correction angle, two extended arms with two holes above and below the osteotomized wedge were, respectively, created (see figure). These two holes were designed not to be initially aligned until the wedge was distracted to the correction angle, as in the preoperative planning. At this moment, an aligning rod was used to pass through the two aligned holes, to assist the surgeon in determining that the correction angle was achieved. The PSI guide was then manufactured by a commercial 3D printer (Formlabs) using biocompatible resin (Dental SG). Before clinical use, moist heat sterilization was adopted and no visible deformation of the PSI profile was allowed to affect the PSI accuracy.
Results and Discussion: ”The average tourniquet time was about 30 minutes, and blood loss was under 20 ml after wound closure. The errors between preoperative planning and surgical results averaged 4.9% and 4.1%, respectively, in WBL [weight-bearing line] percentage and tibial slope. This was attributed to the well-designed PSI guide. The cutting slot with a specified sawing depth can adjust the orientation of the lateral hinge to a position that is close to preoperative planning.“
Conclusion: ”Instead of using a navigator system, this study integrated 2D and 3D preoperative planning to create a PSI guide that can most likely yield outcomes that are close to the planning. Compared with the navigation system, the use of the PSI guide prevents the requirement of continuous tracking and registration that potentially increases surgical errors and consumes time. The advantages of the PSI guide are that it is time-saving, radiation-reducing, and relatively easy to use and that it is a precise procedure. The precise osteotomy is performed with the PSI guide, and good short-term results are achieved without the use of a navigation system.”
Total Shoulder Arthroplasty
Novel 3-dimensionally printed patient-specific guide improves accuracy compared with standard total shoulder arthroplasty guide: a cadaveric study
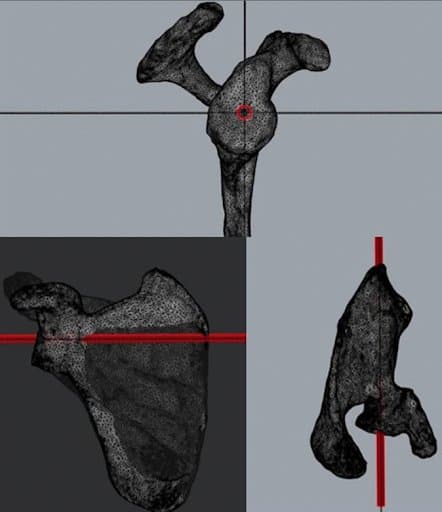
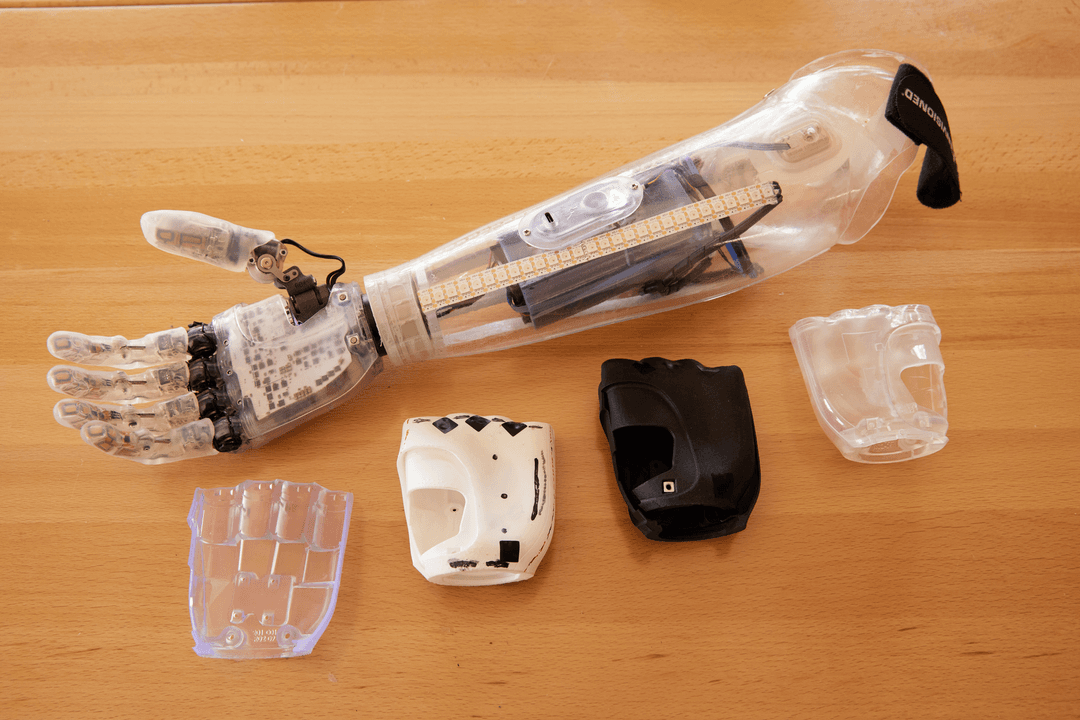
Model of predetermined glenoid guide pin trajectory of 0° of version and 0° of inclination through calculated center glenoid location. Red is a cylinder that simulates placement of the central guide pin.
Design of patient-specific instrumentation device to fit glenoid face. Yellow shape displays the outline of the patient-specific instrumentation guide.
Introduction: “Patient-specific instrumentation (PSI) systems for total shoulder arthroplasty (TSA) can improve glenoid component placement, but may involve considerable expense and production delays. The purpose of this study was to evaluate a novel technique for in-house production of 3-dimensionally printed, patient-specific glenoid guides. We hypothesized that our PSI guide would improve the accuracy of glenoid guide pin placement compared with a standard TSA guide”
Methods and Materials: “We randomized 20 cadaveric shoulders to receive pin placement via the PSI guide (n = 10, study group) or standard TSA guide (n = 10, control group). PSI guides were designed to fit each glenoid based on 3-dimensional scapular models constructed from computed tomography scans. A presurgical plan was created for the guide pin trajectory in neutral version and inclination based on individual scapular anatomy. After pin placement, 3-dimensional models from repeated computed tomography scans were superimposed to calculate deviation from the presurgical plan for each specimen.”
Results: “Inclination deviation was significantly lower in the PSI group than in the standard guide group (1.5° ± 1.6° vs. 6.4° ± 5.0°, P = .009). The glenoid entry site exhibited significantly less deviation in the PSI group (0.8 ± 0.6 mm vs. 2.1 ± 1.2 mm, P = .008).”
“The average total time needed to create each PSI guide from the beginning of surgical planning to post-processing was 4 hours 40 minutes”

Patient-specific device and standard total shoulder arthroplasty guide in use. (A) Patient-specific device with placement of central glenoid guide pin. (B) Standard total shoulder arthroplasty guide in process of placing central glenoid guide pin.
Conclusion: “This study demonstrates a novel technique for in-house production of 3-dimensionally printed, patient-specific devices for TSA central glenoid guide pin placement. These patient-specific guides improved the accuracy of glenoid pin placement based on 3D CT measurements compared with standard TSA guides in a cadaveric model. Our patient-specific glenoid guides can be produced on demand, in-house, inexpensively, and with significantly reduced time compared with commercially available guides.”
Resection of Nonunion and Hindfoot Rearthrodesis
3D Printing Surgical Guide for Nonunion: Technique Tip
Introduction: ”Arthrodesis in the foot and ankle is sometimes an ideal solution for our patients; unfortunately, this procedure does not come without several potential complications that can prove to be challenging… Special attention is paid to the subject of nonunion, as it is one of the most common and challenging adverse outcomes following arthrodesis procedures… Early and aggressive treatment of any arthrodesis complication is essential for good clinical outcomes… However, finding the accurate nonunion plane intraoperatively could be challenging. Through a traditional open approach, in the beginning, nothing but a bone wall is visible, and landmarks are scarce to decide an appropriate cutting plane. Therefore, the only way to begin the resection is by slowly progressing, by “blind” bone excision…”
[In this paper] “We present a technical tip to identify the nonunion plane, by using a customized 3D printed surgical guide for resection and hindfoot rearthrodesis.”
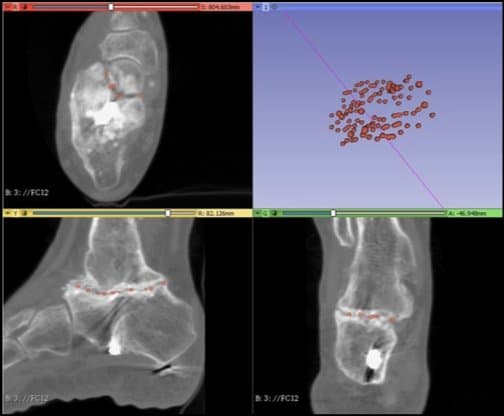
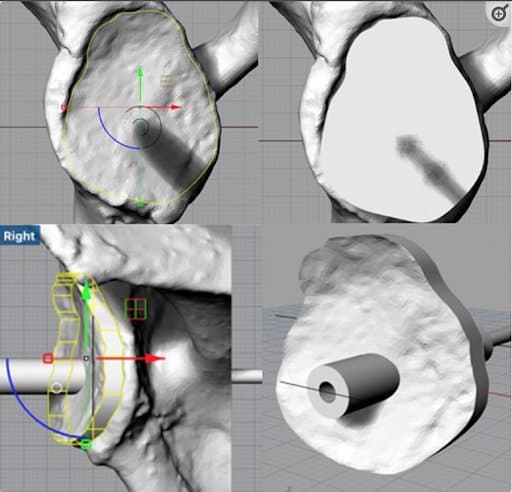
The 3D-nonunion plane is obtained by creating a point cloud. To obtain the point cloud, the nonunion is marked in the 2D CT scan with spheres using axial, sagittal, and coronal views
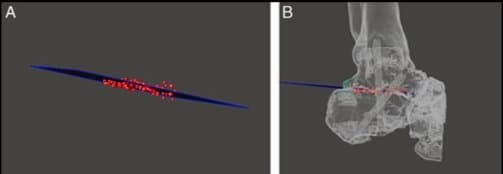
Virtual plane and point cloud in three-dimensional digital model of the foot. A, A virtual plane is drawn to guide the main resection cut based on the point cloud. B, Lateral view.
Materials and methods: Virtual plane and point cloud in 3D digital model of the foot. A, A virtual plane is drawn to guide the main resection cut based on the point cloud. B, Lateral view.
“Once the nonunion plane is obtained, a resection-positioning guide is designed… Since it will be in contact with the patient during the operative procedure, a biocompatible material is needed. Dental LT Clear Resin (FormLabs, MA), with ISO Certificate 134485, is used to print the custom medical device in-house. Subsequently, the resin resection guide is sterilized using ethylene oxide for operative use.”
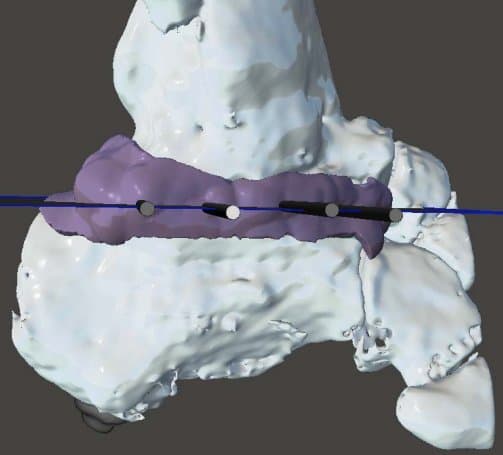
Resection-positioning guide with four cannulated cylinders attached to a template of the lateral aspect of the hindfoot.

3D resection-positioning guide placed over the exposed rim of bone using the anatomic references.
“The plane defined by the K-wires is used to align an oscillating saw and perform the main resection cut, which has an oblique direction from dorsal-lateral to plantar-medial… Compression was achieved at the osteotomy plane and stabilized using an ankle fusion plate”
Discussion: “The use of 3D printing can substantially reduce operative time and the number of fluoroscopy shots… The nonunion planes could be difficult to identify in the operating room, as they are complex spatial deformities. This technique could be helpful as an intraoperative guide, and leads the surgeon to be bone conserving in nonunions that have little real estate on one side.”
Future studies are needed, although the application of this new technique tip in clinical practice in our center brings encouraging results. No complications have been observed yet with this technique tip.”
Conclusion: ”We believe that digitally planned and executed osteotomies facilitated by 3D printed patient-specific guides help the surgeon to minimize human error, improving intraoperative accuracy, while reducing surgical time and intraoperative x-ray exposure, but further studies are needed to determine if this technical tip really improve the clinical results.”
Clavicle Corrective Osteotomies
Virtual Surgical Planning and Mirrored, 3-Dimensional Printed Guides for Corrective Clavicle Osteotomies in Clavicle Malunions and Nonunions
Introduction: “The objective of this study was to retrospectively review clinical and radiographic outcomes of patients who underwent corrective osteotomies for clavicle malunion and internal fixation for nonunion using a combination of virtual surgical planning, patient-specific 3D printed clavicles, and 3D printed cutting guides manufactured at the point of care”
Materials and Methods: ”Between 2015 and 2021, 18 patients underwent corrective osteotomy for a clavicle malunion (7 shoulders) or internal fixation for a clavicle nonunion (11 shoulders)... All patients underwent computed tomography (CT) evaluation of both clavicles. The DICOM files were manually segmented, virtual surgical planning was performed selectively using commercially available software, and a mirrored version of the normal clavicle was 3D printed along with a 3D printed replica of the affected clavicle. 3D printed mirrored clavicles were used in all cases to ensure adequate restoration of the shape and length of the clavicle and to pre-contour fixation plates. Virtual surgical planning (VSP) and 3D printed cutting guides for osteotomy were used in 4/18 (22%) patients… Preoperative, early postoperative, and late postoperative radiographs were reviewed to assess for union and complications. The average follow-up time was 24.9 months.”
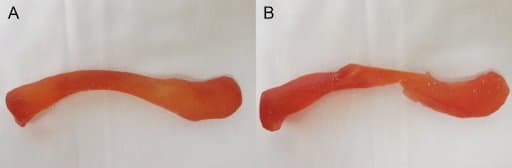
A) 3D printed, mirrored resin model of the uninjured clavicle. B) 3D printed, resin model of malunited clavicle after proposed osteotomy based on preoperative virtual surgical planning.

C) 3D printed cutting guide for corrective osteotomy location and orientation, with slot for saw and holes for Kirschner wire fixation, based on virtual surgical planning. D) Intra-operative photograph of left clavicle with overlain models of both mirrored, native right clavicle and shortened malunited left clavicle.
Results: “Radiographic evaluation at most recent follow-up demonstrated adequate restoration of length and successful union for all shoulders. There were no complications or reoperations. Postoperative patient reported outcomes could be obtained in 16/18 (88.9%) patients… 100% of the patients were satisfied with their outcome (9 very satisfied, 7 satisfied), and their mean subjective shoulder value was 73% (range, 10% to 100%). However, two patients complained of hardware related symptoms, and one patient had return of preoperative symptoms after an interim two years of pain relief.”
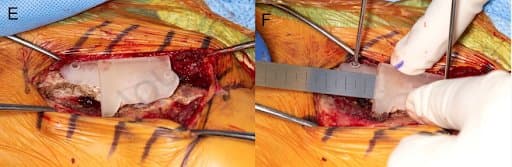
E) Subperiosteally exposed clavicle malunion with cutting guide clipped on. F) Saw being used to create corrective osteotomy through 3D printed guide.
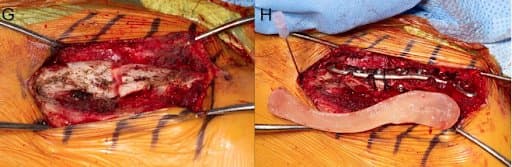
G) View of osteotomy site after cutting guide is removed. H) Final construct with superior clavicle plate augmented by suture cerclage fixation. No intercalary bone graft was used in this patient. Medial end of the clavicle is marked by a spinal needle, with an overlying mirrored 3D model for comparison, demonstrating adequate restoration of native length, alignment, and rotation.
Conclusion: “The use of mirrored 3D printed clavicles combined with VSP and patient-specific 3D guides provides a reliable technique for restoring native anatomy when performing corrective osteotomies for clavicle malunion or internal fixation for clavicle nonunion, with a high rate of satisfactory clinical and radiographic outcomes.”
Comminuted Diaphyseal Fracture Reduction (femur, tibia)
3D printed fracture reduction guides planned and printed at the point of care show high accuracy – a porcine feasibility study
Introduction: “After surgical treatment of comminuted diaphyseal femoral and tibial fractures, relevant malalignment, especially rotational errors occur in up to 40–50%. This either results in a poor clinical outcome or requires revision surgery. This study aims to evaluate the accuracy of reduction if surgery is supported by 3D guides planned and printed at the point of care.”
Materials and Methods: “Ten porcine legs underwent computed tomography (CT) and 3D models of femur and tibia were built. Reduction guides were virtually constructed and fitted to the proximal and distal metaphysis”
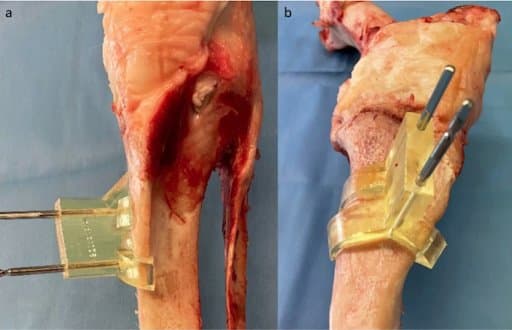
Tibial surgical site with fitted guide.
a) shows the first guide fitted to the medial proximal tibia, fixed with Schanz pins in frontal view
b) demonstrates a closer anteromedial view of the anatomical shaped guide
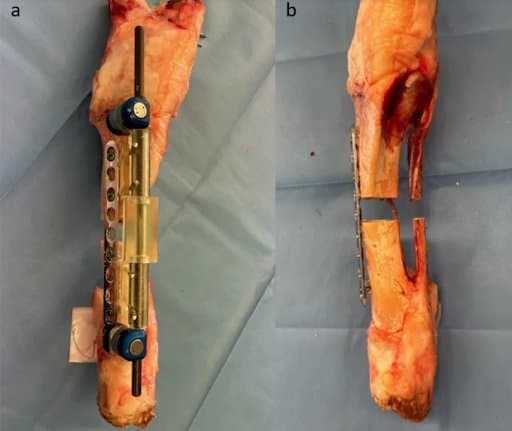
Tibial surgical site after reduction and plate fixation.
a) shows the anteromedial view after plate fixation with the reduction guides and bridging carbon fiber rods still in place.
b) shows final result with the reduction guides and pins removed in the frontal view
“The guides were 3D printed using medically approved resin. Femoral and tibial comminuted diaphyseal fractures were simulated and subsequently reduced using the 3D guides. Postoperative 3D bone models were reconstructed to compare the accuracy to the preoperative planning”
Results: “Femoral reduction showed a mean deviation ± SD from the plan of 1.0 mm ± 0.9 mm for length, 0.9° ± 0.7° for varus/valgus, 1.2° ± 0.9° for procurvatum/recurvatum and 2.0° ± 1.7° for rotation. Analysis of the tibial reduction revealed a mean deviation ± SD of 2.4 mm ± 1.6 mm for length, 1.0° ± 0.6° for varus/valgus, 1.3° ± 1.4° for procurvatum/recurvatum and 2.9° ± 2.2° for rotation”
Conclusion: “This study shows high accuracy of reduction with 3D guides planned and printed at the point of care. Applied to a clinical setting, this technique has the potential to avoid malreduction and consecutive revision surgery in comminuted diaphyseal fractures.”