Source: Formlabs
This blog post features a summary of seven published medical research reports that analyzed the impact of 3D printing in healthcare applications. Here we highlight reports that focus on the impacts of 3D printing in medical education and training.
We maintain a database of hundreds of peer-reviewed publications featuring Formlabs technology. To explore all reports in our database by clinical area and applications, fill out the form below. Or, learn more about Formlabs Medical.
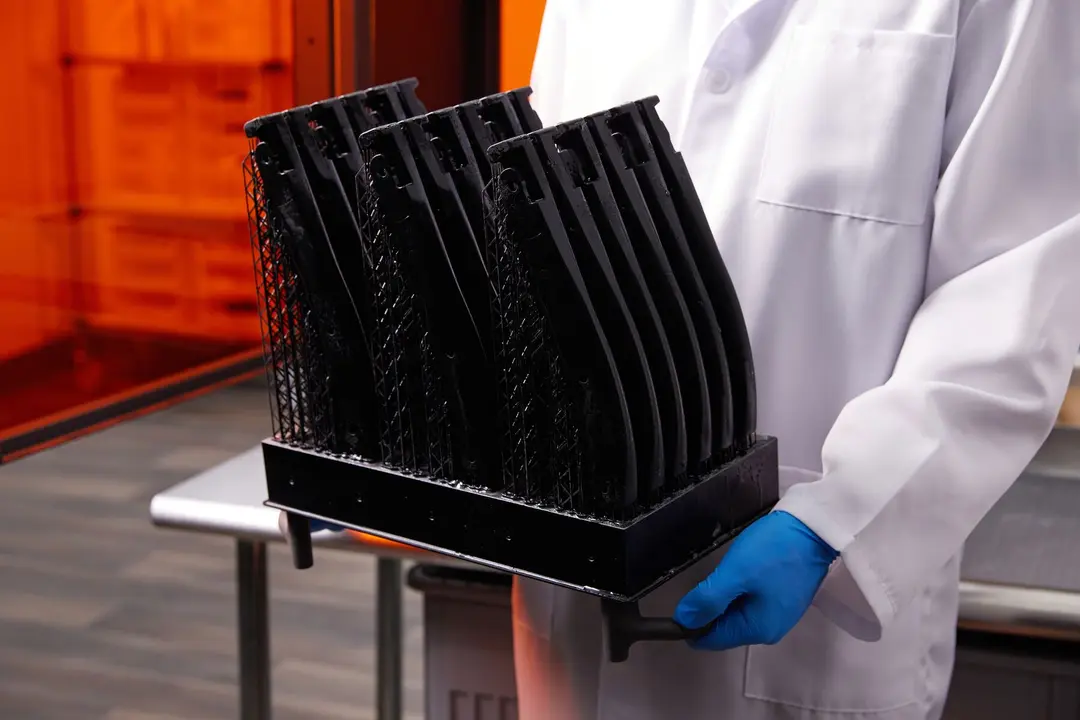
A Simulator for Training in Endovascular Aneurysm Repair: The Use of Three Dimensional Printers
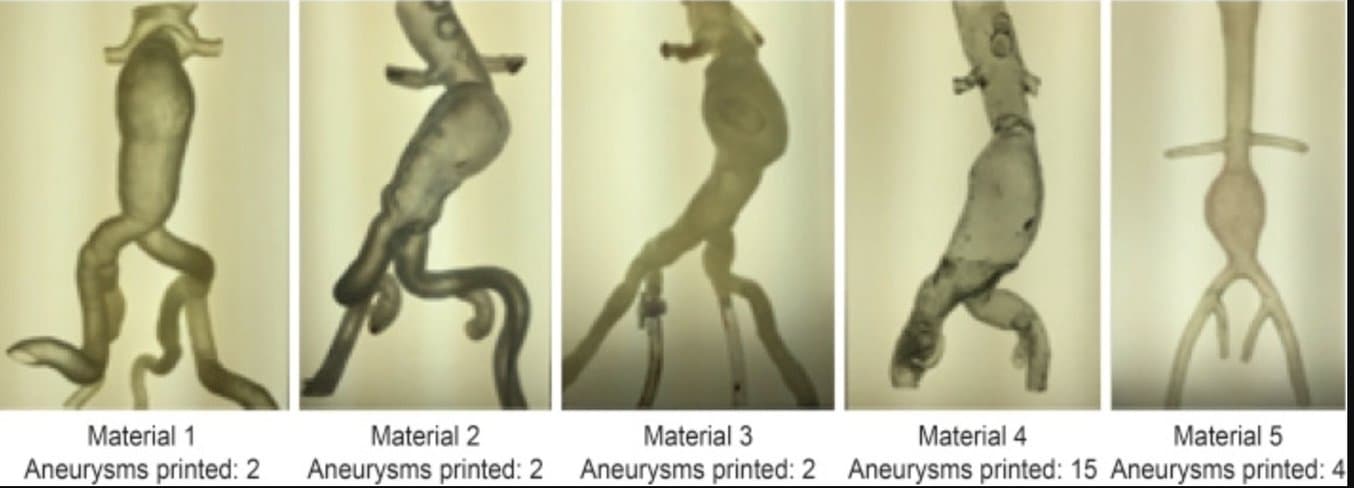
From the report: Steps taken in producing a three dimensionally (3D) printed aneurysm. Note. CT = computed tomography; UV = ultraviolet.
Background: According to the report, “currently, supervised training with progressive exposure to procedures is the norm. However, training based on simulations may shorten the learning curve and avoid exposing patients to unnecessary risks. Attempts at endovascular aneurysm repair (EVAR) simulations date to 1998 with the use of silicone rubber models. Recently, there has been a movement towards computer based simulations. However, these simulations require expensive devices that are prone to technical failure and require regular calibration and maintenance.
Results of this research: Patient specific training reduced fluoroscopy time by 30%, total procedure time by 29%, and volume of contrast used by 25%. The residents reported that the training was useful, realistic, and increased their self confidence. The 3D printers Form1+ (using Flexible Resin) and one from another maker using silicone provided the best performance based on simulator quality and cost.
Note: since this research was completed, Formlabs has launched Flexible Resin 80A and Elastic Resin 50A, offering significant improvements over our original Flexible Resin.
According to the report, “the 3D printers Form1+ (using Flexible Resin)... exhibited the best results based on the quality of the aneurysms (transparency, resistance, and navigability) and cost.”
Citation: I.O. Torres, N. De Luccia, Discipline of Vascular and Endovascular Surgery,
Department of Surgery, São Paulo University Medical School, São Paulo, Brazil (2017). A simulator for training in endovascular aneurysm repair: The use of three dimensional printers.
Evaluation of 3D Printing in Planning, Practicing, and Training for Endovascular Lower Extremity Arterial Interventions
Background: The study, “aimed to investigate the potential role of 3D-printed physical and digital anatomical models in pre-procedural planning, practice and training in lower extremity arterial interventions.”
Results of this research: According to the report, the “measurements obtained from 3D models manually and segmentation images from software were similar (p>0.05). Both were smaller than the actual size of balloons used (p<0.001). Stenosis severity was similar with manual and software methods and both were significantly lower than the reported quantitative angiographic measurements (p<0.001). Vascular access site preference was changed in five (31.2%) patients, when the model was simulated by a non-sterile practice on 3D-printed physical models. The wire and catheter selection differed in eight patients, while practicing with models.
The planning and practicing of lower extremity arterial procedures with 3D models may reduce operator-dependent variables, avoid unnecessary interventions, reduce endothelial damage, and increase procedural success. The 3D-printed models may be used for educational purposes for medical professionals.”
Citation: Göçer, H., Durukan, A. B., Tunç, O., Naser, E., Gürbüz, H. A., & Ertuğrul, E. (2021). Evaluation of 3D printing in planning, practicing, and training for endovascular lower extremity arterial interventions. Turk gogus kalp damar cerrahisi dergisi, 29(1), 20–26. https://doi.org/10.5606/tgkdc.dergisi.2021.20478
The Use of 3D Printers in Medical Education with a Focus on Bone Pathology

Source: Formlabs
Background: The report says that, “the purpose of this study was to determine the feasibility and effectiveness of incorporating three-dimensional (3D)-printed models into pathology lectures. First year medical students with no prior instruction on bone tumors were randomized into two groups: a control group with 2D images and an experimental group with 3D models.”
Results of this research: According to the report, “assessment data showed that although both groups had improved performance and greater confidence post-lecture, those that handled the 3D models had a more favorable experience than those with the 2D images. This study demonstrates 3D-printed models can be incorporated into a pathology lecture and can positively influence teaching-learning outcomes.”
Citation: Youman, S., Dang, E., Jones, M. et al. The Use of 3D Printers in Medical Education with a Focus on Bone Pathology. Med.Sci.Educ. 31, 581–588 (2021). https://doi.org/10.1007/s40670-021-01222-0
Operable, Low-Cost, High-Resolution, Patient-Specific 3D Printed Temporal Bones for Surgical Simulation and Evaluation
Background: The report wanted to know if consumer grade, or desktop 3D printers, could be used to to practice mastoidectomy and to discern mastoidectomy experience level. Typically, professional grade 3D printers required a significant upfront investment, often times of over $100,000.
According to this report, “current models in the literature for mastoidectomy are limited by expense or operability. The aims of this study were (1) to investigate the utility of an inexpensive model for mastoidectomy and (2) to assess whether the model can be used as an evaluation tool to discern the experience level of the surgeon performing mastoidectomy.”
To achieve this, researchers used a CT scan of a seven year old patient and created 3D models which only cost $10 each. Then the report states, “mastoidectomy with facial recess approach was performed by four PGY-2 residents, four PGY-5 residents, and four attending surgeons on the models who then filled out an evaluation. The drilled models were collected and then graded in a blinded fashion by 6 attending otolaryngologists.”
Results of this research: According to the report, “Both residents and faculty felt the model was useful for training (mean score 4.7 out of 5; range: 4-5) and case preparation (mean score: 4.3; range: 3-5). Grading of the drilled models revealed significant differences between junior resident, senior resident, and attending surgeon scores (P = .012) with moderate to excellent interrater agreement (ICC = 0.882).”
Citation: Freiser ME, Ghodadra A, McCall AA, Shaffer AD, Magnetta M, Jabbour N. Operable, Low-Cost, High-Resolution, Patient-Specific 3D Printed Temporal Bones for Surgical Simulation and Evaluation. Annals of Otology, Rhinology & Laryngology. 2021;130(9):1044-1051. doi:10.1177/0003489421993733
Role of 3D Printing and Modeling to Aid in Neuroradiology Education for Medical Trainees
Background: According to radiology.ca, Neuroradiology is a subspecialty of radiology that can be used to help diagnose and treat brain, spine, head, and neck conditions. To aid in the education of neuroradiology, this report stated that, “neuroradiology is a complex subdiscipline of radiology that requires further training beyond radiology residency. This review seeks to explore the clinical value of 3D printing and modeling specifically in enhancing neuroradiology education for radiology physician residents and medical trainees.”
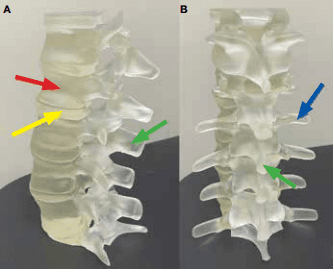
From the report: "A, lateral; and B, posterior views of the lumbar spine. The vertebral bodies (red arrow), spinous (green arrow) and transverse processes (blue arrow), and intervertebral discs (yellow arrow) are all clearly demonstrated.7-9"
Results of this research: “For the purposes of demonstration and proof of concept, 3D-printed objects included a sphenoid bone, cerebellum, skull base, middle ear labyrinth and ossicles, mandible, circle of Willis, carotid aneurysm, and lumbar spine using a combination of clear, white, and elastic resins. Based on this single-institution experience, 3D-printed complex neuroanatomical structures seem feasible and may enhance resident education and patient safety. These same steps and principles may be applied to other subspecialties of radiology. Artificial intelligence also has the potential to advance the 3D process.”
Note: Since this report was published, Formlabs expanded our BioMed Materials library to include BioMed Black Resin and BioMed White Resin.
Citation: Fed Pract. 2021 June;38(6):256-260 | 10.12788/fp.0134, et al. “Role of 3D Printing and Modeling to Aid in Neuroradiology Education for Medical Trainees.” Federal Practitioner, 15 June 2021, https://www.mdedge.com/fedprac/article/241308/neurology/role-3d-printing-and-modeling-aid-neuroradiology-education-medical.
Evaluation of a Modular in Vitro Neurovascular Procedure Simulation for Intracranial Aneurysm Embolization

Source: Formlabs
Background: Developments in endovascular aneurysm therapy creates constant demand for suitable neurointerventional training opportunities. Since it would be affordable and fast to 3D print training environments, this report investigates the value of creating environments in this way.
According to the report, “a large portfolio of 30 patient-specific aneurysm models derived from different treatment settings (eg, coiling, flow diversion, flow disruption) was fabricated using additive manufacturing. Models were integrated into a customizable neurointerventional simulator with interchangeable intracranial and cervical vessel segments and physiological circuit conditions (‘HANNES’; Hamburg ANatomic Neurointerventional Endovascular Simulator). Multiple training courses were performed and participant feedback was obtained using a questionnaire.”
Results of this research: According to the report, the 3D printed training environments were given high evaluations. The report says that, “during a training session, models could be easily exchanged owing to standardized connectors in order to switch to a different treatment situation or to change from ‘treated’ back to ‘untreated’ condition. Among 23 participants evaluating hands-on courses using a five-point scale from 1 (strongly agree) to 5 (strongly disagree), HANNES was mostly rated as ‘highly suitable for practicing aneurysm coil embolization’ (1.78±0.79). HANNES offers a wide variability and flexibility for case-specific hands-on training of intracranial aneurysm treatment, providing equal training conditions for each situation. Moreover, it has the ability to reduce the need for animal experiments.”
Citations: Nawka MT, Spallek J, Kuhl J, et al Evaluation of a modular in vitro neurovascular procedure simulation for intracranial aneurysm embolization Journal of NeuroInterventional Surgery 2020;12:214-219.