Case Study: Patient-Specific Anatomical and Surgical Cutting Guide Models at Yale
In the pursuit of elevating healthcare through innovation, Yale University researchers embarked on a journey to leverage cutting-edge technology to address real-world problems in the orthopaedic space, with the goal of improving clinical outcomes. By harnessing the power of Simpleware software and Formlabs 3D printers, they set out to create CT- and MRI-based patient-specific anatomical models to examine patellar instability [1,2] and surgical cutting guide models to examine the accuracy of surgical guide wire placement for femoral neck stabilization [3]. Using both Simpleware and Formlabs technologies allows researchers to offer personalized care through customized anatomical modeling and surgical guide design, improving both clinical outcomes for patients and procedural efficiency for the healthcare provider. This case study covers how:
-
3D technology can be used to address real-world orthopaedic problems to study patellar instability and femoral neck stabilisation.
-
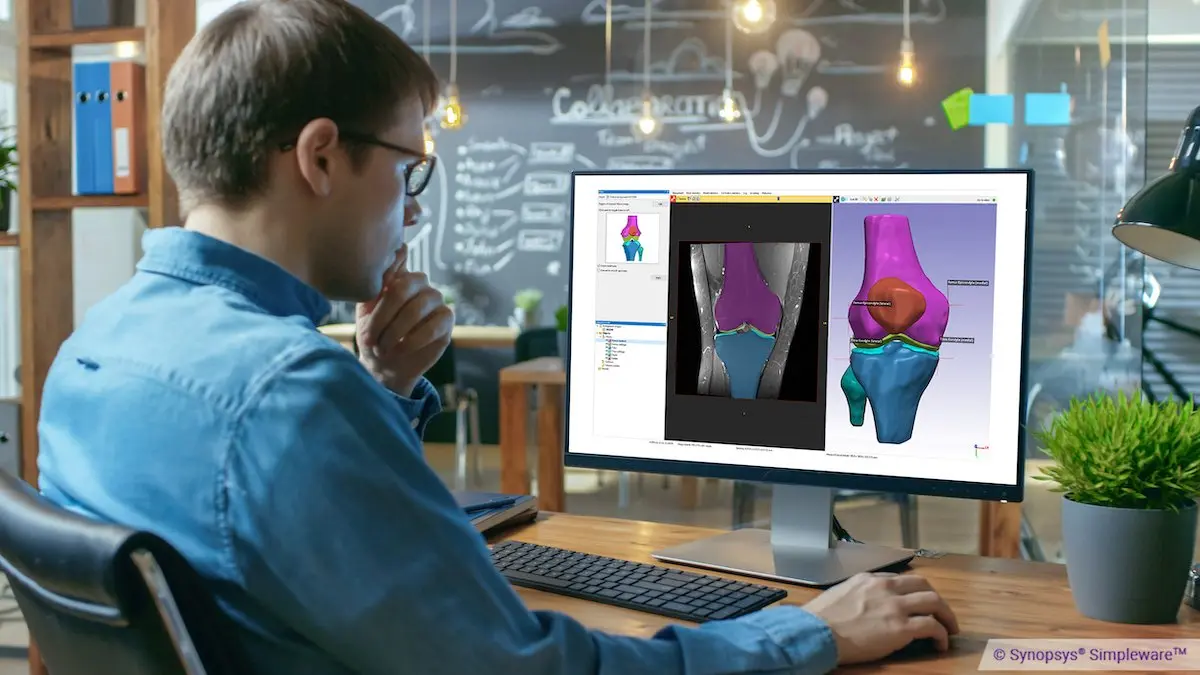
Synopsys Simpleware software can be used to generate patient-specific anatomical models and to analyze CT scan data via measurements and deviation analysis.
-
3D printed models from Formlabs can help plan and guide complex interventions.
-
Workflows combining these technologies offer great potential for improved personalized medicine.
“At Yale University, we needed a software solution that could span the School of Medicine as well as the School of Engineering. Simpleware allows us to process CT or MRI based imaging to develop highly accurate anatomic models and import them into finite element models, conduct surgical planning, print personalized surgical guides and advance our clinical research.”
Creating Bone Simulation Models for Cutting and Drilling
3D printed bone-simulation models are revolutionizing medical training, surgical planning, research, and medical device development. This application guide walks through the bone-simulation material options for stereolithography (SLA) 3D printing and the entire in-house manufacturing process for bone-like anatomical models intended for cutting and drilling.
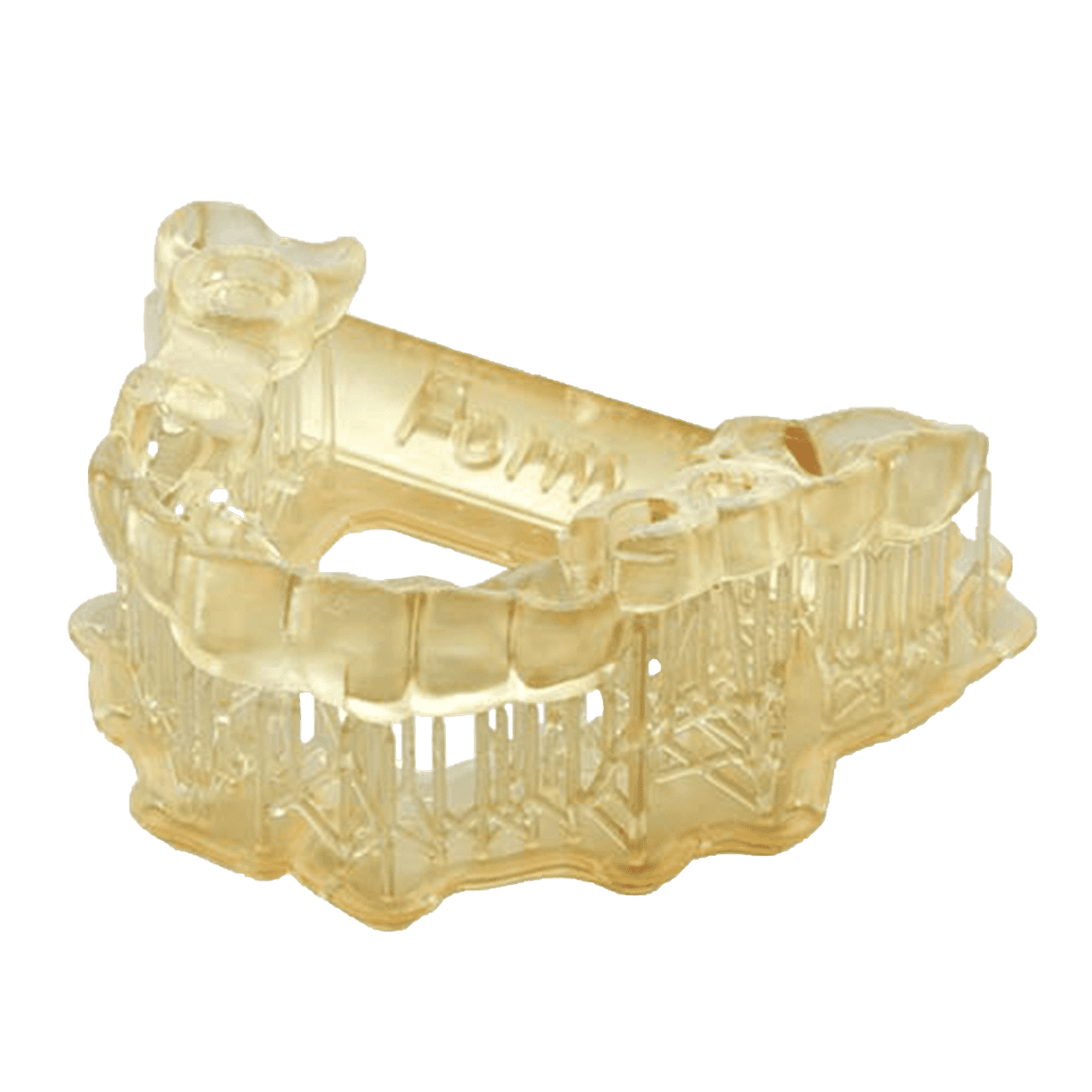
Patient-Specific Surgical Guide 3D Printing
The main aim in femoral neck stabilisation is to reduce the health risks associated with fractures. There are three potential methods to fix these fractures — using three screws, the Synthes Femoral Neck System (FNS), or a dynamic hip screw (DHS). However, all these methods require precise positioning of guide wires to place the implants correctly in the femoral neck and head. Getting this positioning consistent and accurate is crucial to shorten surgery times, effectively stabilise fractures, and lower the chances of complications. To speed up surgeries and ensure the best implant placement, especially for elderly patients, the researchers developed and tested a surgical planning approach using 3D modelling and stereolithography (SLA) 3D printing technology.

Personalized Surgery With 3D Printing
Watch our medical 3D Printing Q&A with 3D LifePrints to discover their innovative and versatile work creating patient-specific medical devices.
Description of Workflow
Synopsys Simpleware software was used to create 3D virtual surgical models to place guide wires in a model of an osteoporotic proximal femur Sawbone. “At Yale University, we needed a software solution that could span the School of Medicine as well as the School of Engineering. Simpleware allows us to process CT or MRI based imaging to develop highly accurate anatomic models and import them into finite element models, conduct surgical planning, print personalized surgical guides and advance our clinical research,” says Dr. Daniel Wiznia.
Three different guides were designed to optimise implant placement for each of the three implant systems; they were then 3D printed using a Form 3 SLA 3D Printer from Formlabs.
A trauma fellowship-trained orthopaedic surgeon used these 3D printed guides to position drill bit tipped guidewires into five fragile hip bone models for each of the three systems, for a total of fifteen bone models.
CT scans of each bone model with the implants in place were then taken and Simpleware software was used to process the 3D images and measure the displacement and angular deviations at guide wire entry to the optimal Sawbone model.
Results and Discussion
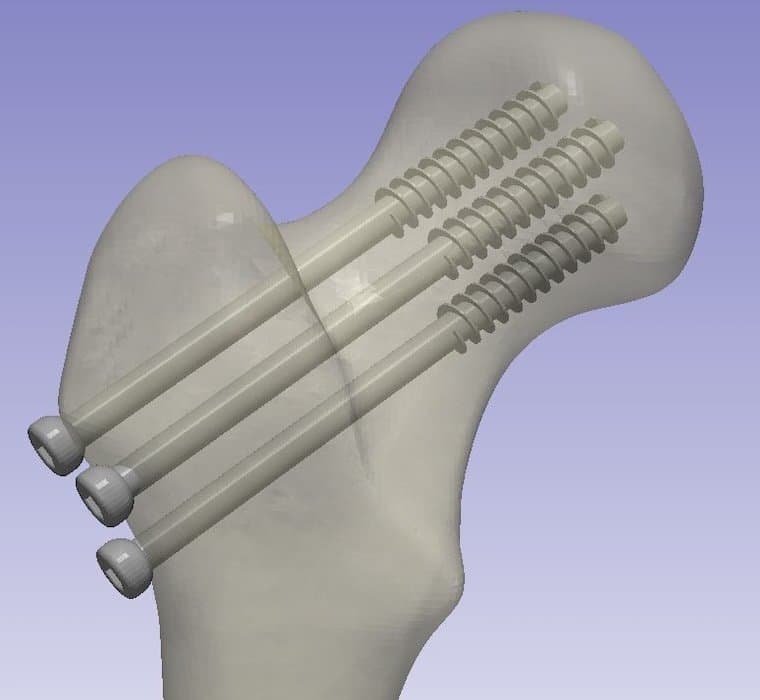
A virtual 3D surgical model for guide wires.
-
Percutaneous screws: Displacement 3.19 mm (±0.12), Angular deviation 4.10° (±0.17)
-
Femoral Neck System: Displacement 1.59 mm (±0.18), Angular deviation 2.81° (±0.64)
-
Dynamic Hip Screw: Displacement 1.03 mm (±0.19), Angular deviation 2.59° (±0.39)
The custom 3D printed drill guides proved accurate in guiding the placement and angular positioning of guide wires for stabilising hip fractures.
The use of multiple guide wires resulted in diminished positional accuracy and increased angular deviation, possibly due to cumulative guide shifting during wire placement. Notably, the percutaneous screw system drill guide exhibited relatively lower accuracy compared to the other two guides, likely attributable to its requirement of three wires, potentially causing slight guide shifting during wire insertion.
The researchers were able to refine their guide design iteratively, which proved instrumental in enhancing guide strength and accuracy. Key insights encompassed optimising guide wire channels for sufficient length to ensure stability and prevent breakage during drilling, as evidenced by the turret design in the final two iterations. Additionally, leveraging anatomical features like the greater trochanter and metadiaphyseal and diaphyseal shafts as secure attachment points for the guides proved crucial.
Conclusions
The authors presented a comprehensive study describing how to develop and validate a surgical planning methodology using 3D modelling and printing technology, which will help expedite surgery and achieve ideal implant positioning.
The custom 3D printed drill guides provided for a robust accurate application of percutaneous screw, FNS, and DHS systems’ guide wires. Drill guides used in the placement of more than one guide wire were found to have a lower relative positional accuracy. This work, along with the iterations of guides that they completed, will inform future development of drill guides for use in cadaveric models and, ultimately, personalized, and tailored treatment for patients who require femoral neck stabilization.
Request a Free Sample Part
See and feel Formlabs quality firsthand. We’ll ship a free sample part printed in Sugical Guide resin to your office.
Anatomical 3D Printing from MRI and CT
Yale researchers employ 3D printing to assess joints.
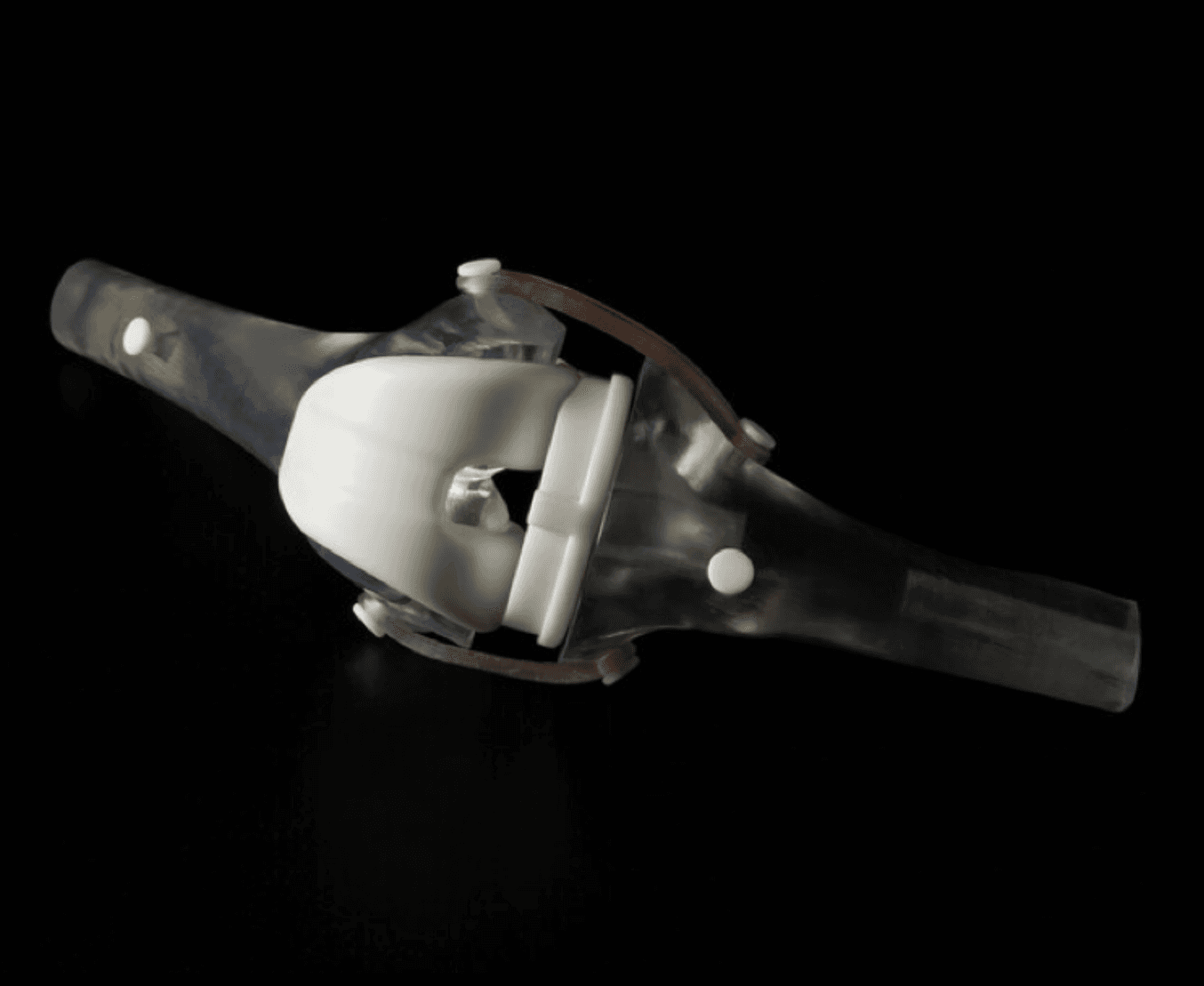
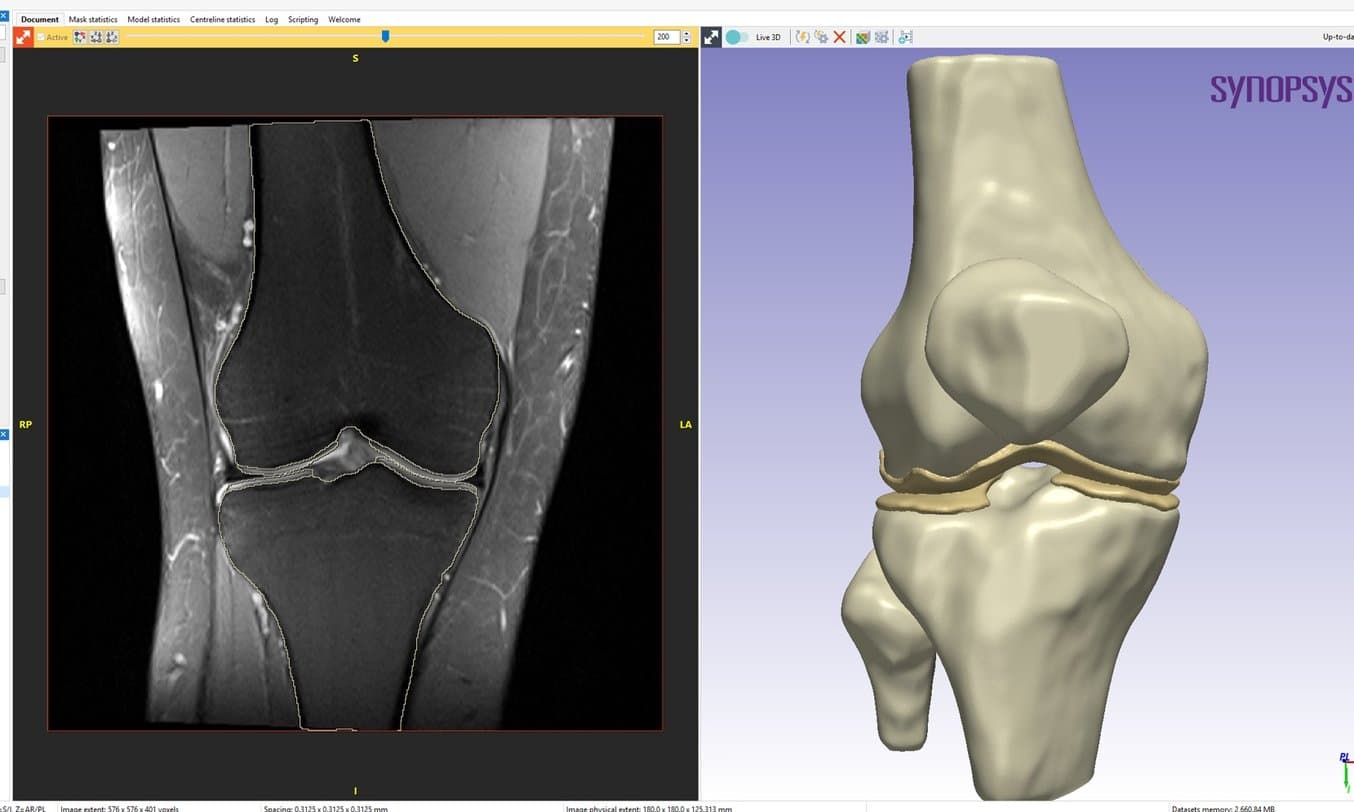
Three-dimensional (3D) modelling is widely utilised in various orthopaedic subspecialties such as spine surgery, trauma, oncology, and arthroplasty. However, knee surgery has traditionally relied on conventional imaging modalities like X-ray, MRI, and CT, largely overlooking the potential of 3D modelling and 3D printing. Understanding trochlear dysplasia is pivotal for surgical planning in patellar instability cases, but surgeons currently rely on 2D metrics to comprehend the intricate 3D deformities involved. As an emerging trend, more studies are employing 3D printing to assess the patellofemoral joint. In these two methods papers from Yale University, they elaborate on techniques for 3D printing anatomical models and demonstrate their utility in preoperative planning for patients with patellar instability. CT scans were used to generate models of the bony structures of the knee, and MRI scans were used to generate models of the articular cartilage in the patellofemoral joint.
Description of CT and MRI Based Workflow
The workflow used for the CT and MRI-Based studies are nicely outlined in videos provided by the authors of the studies:
CT scans of the knee were obtained in an upright, weight-bearing CT scanner in a standing position and then at 20° of flexion position. The authors point out that the protocol used in this case study can also be applied to more traditional supine CT scanners.
MRI scans of the knee were obtained using a custom thin section sagittal gradient echo MRI sequence, which maximises the accuracy of the 3D model produced using MRI data as it maximises the difference in image intensity between cartilage and other soft tissue.
The DICOM files were then imported into Synopsys Simpleware ScanIP software (Synopsys Inc., Sunnyvale, CA) to convert medical imaging data into 3D models using a combination of automated and manual techniques. Although the MRI-based segmentation workflow was similar to the CT-based workflow, the MRI process tends to be more manual due to decreased contrast in the image greyscale gradients and the non-cubic image voxels. Therefore, more care and time must be taken to ensure accurate segmentation and model generation.
Once the mask is checked for accuracy, it was optimised for printing by filling its internal structure; the surface is then embossed with a patient identifier before being exported as an STL file.
For 3D printing, a Form 3B or Form 3BL printer was used, which can print with submillimeter resolution. The STL was imported into PreForm software (Formlabs), to prepare the material resolution, scale, print orientation, and density of support structures.
Once the printing process was complete, the finished model was removed from the printer and washed in isopropyl alcohol for 20 minutes in a Form Wash system. After drying, the print underwent a post-cure process in which it was exposed to ultraviolet light for 30 minutes at 60 °C in a Form Cure system. Finally, the support material was removed carefully with hand tools and the print was ready to be analyzed.
Note: The researchers have recently started using the Simpleware AS Ortho add-on module, an automated AI-enabled segmentation tool (link), and although it was not applied to the current study, we look forward to seeing the results of current and future studies that will be able to leverage the technology.
Discussion and Conclusion
The authors presented a comprehensive methodology for generating 3D printed models of the patellofemoral joint. This method encompasses CT and MRI image acquisition, image segmentation, model generation, and 3D printing. These models serve as valuable tools to aid surgeons in enhancing their understanding and planning of surgical interventions for recurrent patellar dislocations.
Trochlear dysplasia, a complex 3D deformity associated with patellar instability, can also be better understood through 3D reproductions of dysplastic geometry and trochlear tracking paths. This approach enables better understanding of trochlear curvatures, entry points for the patella, and lateral alignment for surgical planning. “We’ve been very impressed with the customization and automation features,” says Dr. Wiznia.
Furthermore, the potential of 3D modelling extends beyond this method, offering valuable insights for patellofemoral surgery planning. Three-dimensional images and prints provide a comprehensive view of trochlear groove characteristics and their relation to patellar instability, aiding in surgical design and understanding deformities in other cases. “We’ve been able to share the software across the University campus with multiple labs and clinical environments, as well as integrate the software into our undergraduate and graduate school curriculums,” says Dr. Wiznia.
Learn more about how 3D printing can be used for medical applications and explore Formlabs’ range of biocompatible medical materials.
Reference
-
Beitler BG et al. Three-Dimensional Printing of the Patellofemoral Joints of Patellar Instability Patients. Arthrosc Tech. 2023 Feb 27;12(3) https://www.sciencedirect.com/science/article/pii/S2212628722003073
-
Beitler BG et al. Three-Dimensional Printing of Models of Patellofemoral Joint Articular Cartilage in Patients With Patella Instability for Observing Joint Congruity. Arthrosc Tech. 2023 Sep 25 https://www.sciencedirect.com/science/article/pii/S2212628723001901
-
Roytman GR et al. Accuracy of guide wire placement for femoral neck stabilization using 3D printed drill guides. 3D Print Med. 2022 Jul 4;8(1):19. https://threedmedprint.biomedcentral.com/articles/10.1186/s41205-022-00146-8/


