Formlabs would like to thank Dr. Jonathan Morris, Ms. Amy Alexander, Dr. Jane Matsumoto, and others from the Mayo Clinic Anatomic Modeling Unit and Department of Engineering for their pioneering work, research, mentorship, and volunteerism in this space.
Developing a POC Manufacturing Program for CMF
Introduction: “Virtual surgical planning (VSP) and three-dimensional (3D) printing have been transformative in craniomaxillofacial surgery where preoperative planning and the fabrication of patient-specific cutting guides and implants have led to a more accurate and efficient reconstruction of geometrically complex anatomic defects with a decrease in intraoperative decision making and reduction of surgery time.”

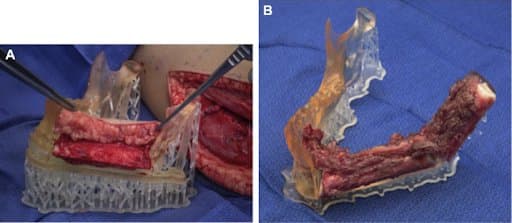
POC 3D printed cutting guides and modified anatomic models for resection of maxillary sinus tumor and reconstruction of hemimaxillectomy defect with a free fibula flap.
The paper further discusses sections about funding, physical space (for printing within a hospital), the importance of information technology support and the confidentiality with electronic health records.
“The process of generating 3D objects from a digital blueprint is described as follows: (1) image acquisition, (2) extraction of the regions of interest (segmentation), (3) transformation of the data from volumetric to a 3D triangular mesh, (4) digital planning of surgical intervention, (4) conversion of data into one of many files (Standard Tessellation Language [STL], OBJ, VRML, or 3MF file), (5) transfer of the data to a 3D printer for production, (6) cleaning, sterilization and inspection of the models and/or devices, and (7) quality control of the models.”
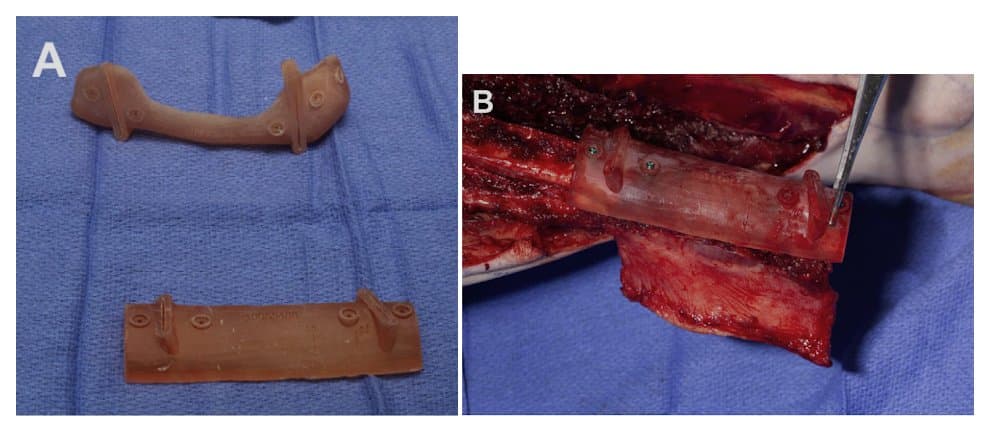
(A) POC 3D printed mandible resection and fibula osteotomy guides
(B) Fibula osteotomy guide secured before contouring osteotomies
The paper also comments on different printing technologies. “Powder bed fusion and vat photopolymerization may be used for fabrication of models, surgical tools, patient-specific implants (PSIs), and tissue engineering scaffolds....The group of materials with the largest versatility in 3D printing is the polymer-based materials. They can be used in the fabrication of bioengineering scaffolds and surgical guides, and the design of drug delivery vehicles.”
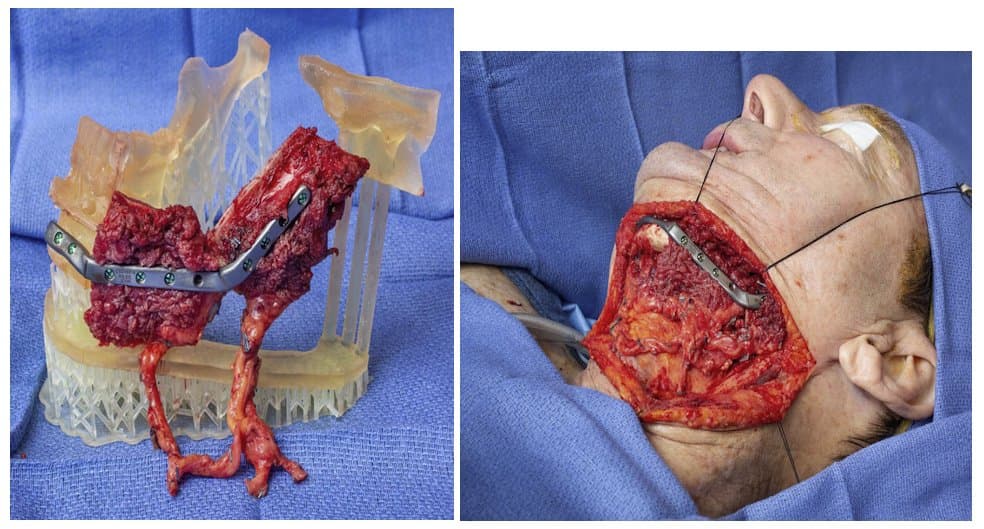
Photo One (left): Patient-specific fixation tray used for fixation of scapula flap at the side table before transfer to the head and neck region
Photo Two (right): Inset of chimeric scapular free flap at the head and neck region.
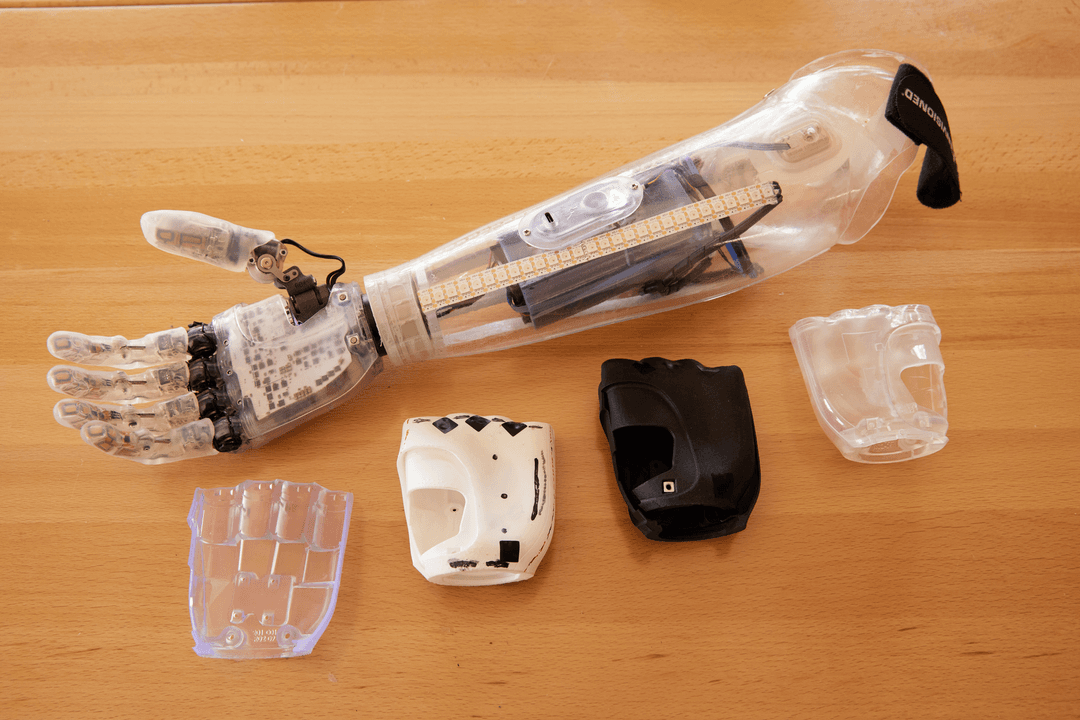
The authors describe their own experience with Point-of-care manufacturing in craniomaxillofacial surgery and share illustrations of different clinical cases. Formlabs BioMed Amber Resin was used for the creation of all 3D-printed parts. BioMed Clear Resin could also be considered for those looking to create similar parts.

Posttreatment CT scan with 3D reconstruction of chimeric scapular free flap reconstruction of mandibular defect.
Short and Long-term Outcomes of Three-dimensional Printed Surgical Guides and Virtual Surgical Planning Versus Conventional Methods for Fibula Free Flap Reconstruction of the Mandible: Decreased Nonunion and Complication Rates
Background and methods: The aim of this retrospective study (years 2010-2018) was to determine whether virtual surgical planning and 3D printed cutting guides improved radiographic bone union compared to conventional methods in fibula free flap reconstruction of the mandibles. Osseous union was evaluated by a radiologist blinded to each patient's treatment. 260 patients were included.
Results and Conclusions: Bony union was achieved in 96% of patients with VSP and 3D printed guides (compared to 80% in the conventional group). Complication rate was significantly lower in the 3D/VSP group (11% compared to 38%), and median time to bony union was significantly shorter (0.8 years compared to 1.4 years) than in the conventional group.
“Therefore, 3D/VSP reduced the rate of radiographic nonunion and flap-related complications in FFF reconstruction for mandibular defects.”
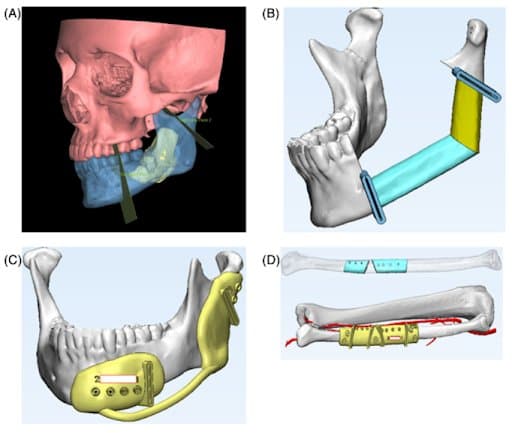
VSP with computer aid design of 3D printed cutting guides. CT imaging is segmented to anatomically outline soft tissue, bone, and tumor. Precise osteotomy sites are planned for a customized treatment plan (A). Angulation and length of fibular segments is optimized for form and function of FFF inset (B). Customized cutting guides are designed for both mandible and fibula segments (C, D).
Novel Patient-Specific 3-Dimensional Printed Fixation Tray for Mandibular Reconstruction With Fibular Free Flaps
Fixation tray used at the donor site to confirm fit of the fibular segments after osteotomy is performed.
Background: “Segmental mandibular defects can be debilitating because of their impact on function and facial aesthetics. The free fibular flap for mandibular reconstruction is well documented and remains a commonly used flap because of its bone length, versatility, distant location from the head and neck region that allows for a 2-team approach, and ability to simultaneously place endosseous implants. Virtual surgical planning and patient-specific cutting guides have facilitated complex 3-dimensional (3D) reconstruction.
The goal of this report is to describe the authors' experience with the use of a novel 3D printed fixation tray.”
Conclusions: “The fixation tray provides dual functionality by aiding in alignment and stabilization of the fibular segments and concomitantly providing patient-specific anatomic references for indexing of bony and soft tissue components. This tray enables rapid ex vivo configuration of the fibula segment(s) with the reconstruction bar relative to the native mandibular segments and allows the compiled construct to be transferred to the head and neck for insetting as a precisely configured single unit. The ability to relate the segments to one another without soft tissue encumbrances greatly enhances the ability to align the segments accurately and the authors have found that it also greatly shortens the amount of time needed for insetting of the flap.”
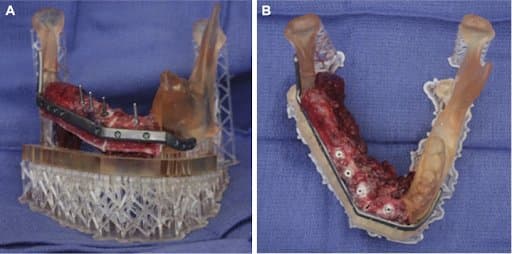
Right mandibular body and symphysis segmental defect. A, Inset of fibular flap and osteotomies for immediate implant placement and confirmation of angulation. B, Bird's eye view of reconstruction after immediate implant placement.
Quality Assurance and Printing Accuracy Analysis of 3D Printing in Medical Applications
Introduction: “Despite its recent introduction into clinical medical practice, three-dimensional (3D) printing is having a significant impact on patient care…. However, there is a lack of standardization, particularly in terms of quality assurance (QA) to ensure that the 3D printed model accurately represents the corresponding patient’s anatomy and pathology…. In this study, we investigated printing accuracy on a diverse selection of 3D printers commonly used in the medical field.”
Methods: “A specially designed 3D printing QA phantom was periodically printed on 16 printers used in our practice, covering five distinct printing technologies (material jetting, vat photopolymerization, material extrusion, binder jetting, and powder bed fusion) and eight different vendors. Longitudinal data were acquired over a period of six months with the QA phantom printed monthly on each printer. Qualitative assessment and quantitative measurements were obtained for each printed phantom.”
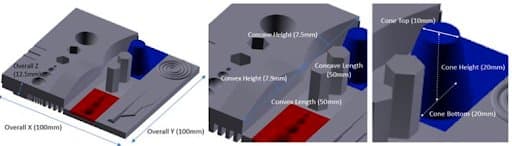
QA phantom used in this study includes various geometric and anatomic structures (it also had features such as a vascular tree and cochlear spiral to simulate fine anatomical structures).
Results: “The mean printing error for all printers ranged from -1.75 mm to 0.55 mm (Table 2, negative values indicate under- printing while positive values indicate over-printing). Most of our 3D printers were reasonably accurate, with printing errors within ± 1 mm. Two printers, NP1 and EOS P110, had mean errors larger than ±1 mm, both under-printing (-1.18 and -1.75 mm). The NP1 printer had a printing error beyond ±1 mm 14 different times across all 60 measurements. The EOS P110 printer produced errors beyond ±1 mm twice, with one of those times being a significant outlier. In this outlier measurement, the printing error was -11.86 mm on a dimension with a truth value of 20 mm. The HP-580 printer had a printing error beyond ±1 mm twice as well. The Ultimaker A printer was beyond ±1 mm 6 times, and the ProJet printer was beyond ±1 mm once.”
“There was a lack of surface and curvature smoothness for the convex portion of phantoms produced by the material extrusion printers. The Ultimaker printers struggled with curvature smoothness and consistently failed the hex portion fit test. The PRUSA printer struggled with surface smoothness and always produced only 3 out of 4 branches in the vascular tree. There were problems observed in phantoms printed by the powder bed fusion printers as well. For phantoms printed by HP-580, there were consistent raised edges on the positive features of the phantom as well as wrinkles on the sides and back faces. Wrinkled surfaces were also present on phantoms printed by the EOS P110 printer.
Trends: “Overall, considering both quantitative and qualitative data, we found that our material jetting and vat photopolymerization printers were the most accurate.
…The data also showed that there were noticeable differences in accuracy between printers of the same printing technology but from different vendors. This difference was seen between our Formlabs printers and our NewPro NP1. The percentage error (printing error divided by the true value, multiplied by 100) of NP1 was 7.8 times higher than the Formlabs printers.”
Conclusion: “This study has demonstrated that the accuracy of 3D printing depends on the printing technology, manufacturer, and model… As new printing technologies and advancements are introduced, it is crucial to be aware of the varying accuracy we discovered due to the possible detrimental consequences of inaccuracies when 3D printed objects are used in surgery, pre-operative planning, custom medical device creation, and the impactful applications to come.”