Left Atrial Appendage Closure Guided by 3D Computed Tomography Printing Technology: A Case Control Study
Introduction
“We sought to evaluate the additional value of left atrial appendage (LAA) 3D printing derived from computed tomography (CCT) in determining the size for LAA occlusion (LAAO) devices as compared to standard measurement by using occurrence of LAA leak as endpoint.”
Methods and Materials
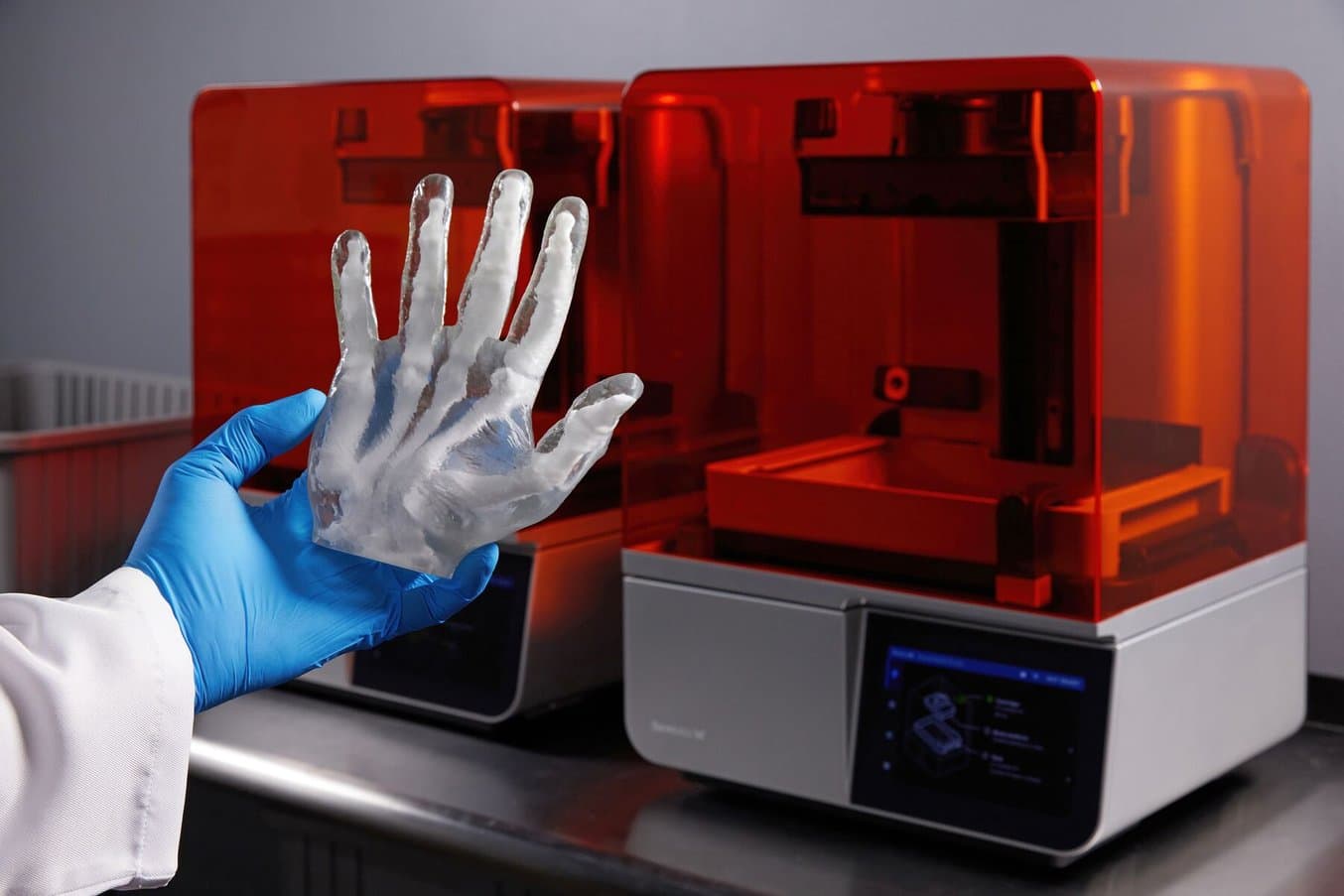
In this pilot, a retrospective case-control study “we evaluated 6 patients with LAA leak (cases) and 14 matched patients without LAA leak (controls) after LAAO. All patients before the LAAO procedure underwent CCT and TEE. The LAAO procedure was performed with TEE and cardiac angiography (CA) monitoring and the sizing of the device was decided on the basis of TEE, CCT, and CA. For each group, a patient-specific 3D printed model of LAA was manufactured using CT pre-operative images. The model was finally 3D printed using a Form 2 Desktop printer* (Formlabs Inc., MA, USA), based on vat-photopolymerization technology. The LAA landing zone was then measured manually by a digital caliper. Visual inspection of the LAA occluder apposition was used to confirm the selection. Finally, the size recommended by the 3D printed model was compared with the size of the implanted device to assess agreement, overestimation, or underestimation and its relation with post-operative leak.”
*The latest version of the Form 2 stereolithography SLA 3D printer is the Form 3+.
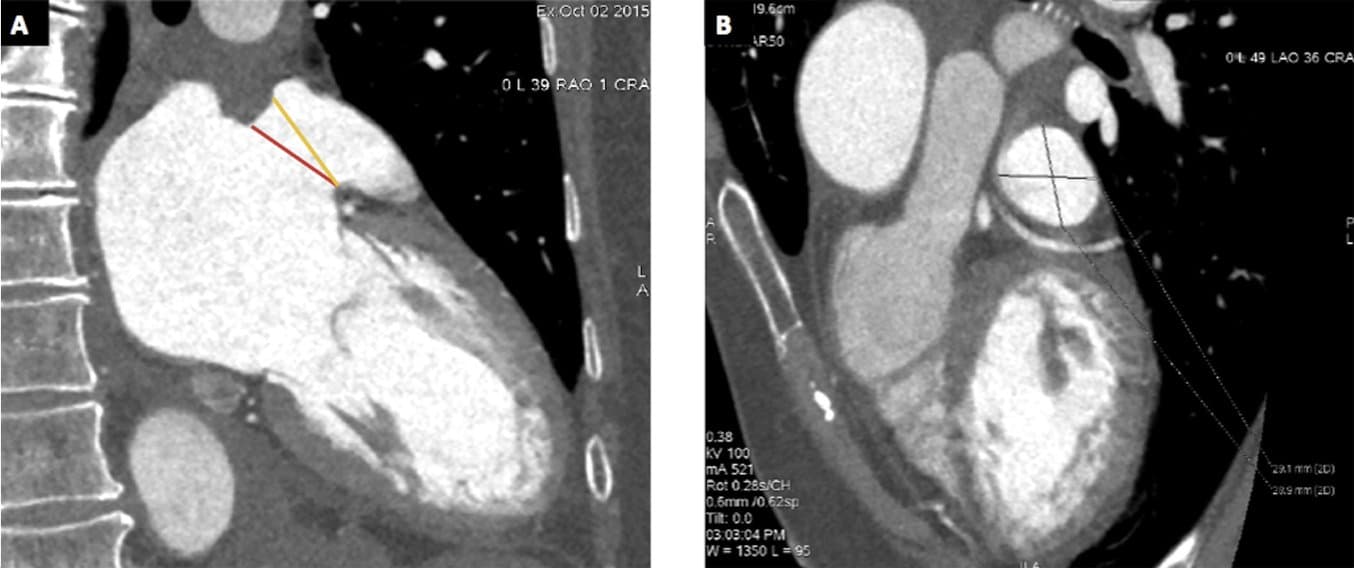
A: CCT measures of ostium (red line) and landing zone (yellow line) in 2 chamber view. Panel B: CCT image showing the measures of the show axis view of the landing zone.
Formlabs Biocompatible Resins: A Comprehensive Guide To Choosing the Right Material
Formlabs currently offers more than 40 unique materials for stereolithography (SLA) 3D printing. This paper helps users compare and contrast our biocompatible offerings, and determine the best fit for their medical applications.
Results
“The comparison of the implanted prosthesis size versus the sizing performed by the 3D printed model showed underestimation in 11 patients (55%), agreement in 7 patients (35%), and overestimation in 2 cases (10%)... The prevalence of LAA leak was significantly higher in the subset of patients with underestimation of prosthesis implanted (6 out of 11 patients vs 0 out of 9 patients, p = 0.019).”
Discussion
“Using LAA leak as the primary endpoint, 3D-printed models of LAA derived from CCT appear more accurate for sizing of LAAO compared to standard evaluation based on pre-operative TEE, CCT, and CA independently by the implanted device.”
Conclusion
“3D printing of the LAA derived from CCT is feasible and may add value to CCT, TEE, or CA derived LAAO device prosthesis sizing by reducing LAA leak.”
Citation: Michele Conti, Stefania Marconi, Giuseppe Muscogiuri, Marco Guglielmo, Andrea Baggiano, Gianpiero Italiano, Maria Elisabetta Mancini, Ferdinando Auricchio, Daniele Andreini, Mark G. Rabbat, Andrea Igoren Guaricci, Gaetano Fassini, Alessio Gasperetti, Fabrizio Costa, Claudio Tondo, Anna Maltagliati, Mauro Pepi, Gianluca Pontone, Left atrial appendage closure guided by 3D computed tomography printing technology: A case control study, Journal of Cardiovascular Computed Tomography, Volume 13, Issue 6, 2019, Pages 336-339, ISSN 1934-5925, https://doi.org/10.1016/j.jcct.2018.10.024
Application Guide: Printing Soft Anatomical Models Using BioMed Flex 80A Resin and BioMed Elastic 50A Resin
This guide aims to help the user decide on the best method of silicone part production for their intended use, and provides step-by-step instructions for both printing with Silicone 40A, and molding silicone using SLA 3D printed tooling (including two-part injection molds, overmolds, and compression molds).
3D-Printed Models for Left Atrial Appendage Occlusion Planning: A Detailed Workflow
Introduction
“Left atrial appendage occlusion (LAAO) is a structural interventional cardiology procedure that offers several possibilities for the application of additive manufacturing technologies. The literature shows a growing interest in the use of 3D-printed models for LAAO procedure planning and occlusion device choice. This study aims to describe a full workflow to create a 3D-printed LAA model for LAAO procedure planning.”
Methodology/Approach
“In addition to the diagnostic image acquisition, the workflow is composed of three principal steps: image segmentation, 3D modeling, and 3D printing…
"Different additive manufacturing technologies and materials were analyzed to identify which provided the best response to the medical equip requests of model flexibility, transparency, and cost efficiency in a preliminary phase of the activity. Polyjet technology (Stratasys, Eden Prairie, MN) and Formlabs (Formlabs; Somerville, MA) Stereolithography (SLA) were considered the most promising among all other processes….Specimens of different Polyjet Cardiac materials were printed with a J850 Digital Anatomy Printer and compared with Formlabs Form 3B+ 3D Printer Elastic 50 A specimen. The medical equip judgment was in favor of SLA; flexibility and haptic response were considered similar for the two different technologies, but SLA prints demonstrated superior transparency and an inferior cost.”

Left atrial appendage model
“The models are printed using a Formlabs 3B+ SLA 3D printer in transparent Elastic 50 A material. The print process takes an average of 6.5 h for each model with an average volume of 12.8 ml of material per model. The printer allows printing up to four different models at the same time, reducing the overall total print time to about 9 h.”
Findings
“Models produced with the described workflow have been used at the Careggi Hospital of Florence as LAAO auxiliary planning tool in 10 cases of interest, demonstrating a good correlation with state-of-the-art software for device selection and improving the surgeon’s understanding of patient anatomy and device positioning.”

Amplatzer Amulet device positioning on 3D-printed model
Discussion
“The advantages of 3D printed models in the planning of SHS procedures, and specifically of LAAO interventions, are already acknowledged in dedicated medical literature (Bartel et al., 2018; DeCampos et al., 2022; Fan et al., 2019; Oliveira-Santos et al., 2019; Wang et al., 2018). The present work does not investigate further in these benefits, but is meant to describe how to create 3D printed models fit for the purpose.”
“... the 3D models created following the procedure described were used and appreciated by the medical equip to improve the understanding of patient anatomy, especially in difficult cases like retroverted or bi/trilobed LAA, and the positioning of the device in the landing zone.”
“In detail, the medical equip was satisfied with the haptic feedback of the material, considered suitable to represent the LAA tissue behavior. The flexibility of the model was hence deemed useful to simulate the actual positioning of the device in the LAA neck and ostium. The transparency of the model was considered helpful in the visualization of the spatial position of the device and its spatial proportion with the surrounding anatomical structures.”

Watchmen FLX positioning on 3D printed model
Originality/Value
“3D-printed models for the LAAO planning are already described in the literature [references are found in original article]. The novelty of the article lies in the detailed description of a robust workflow for the creation of these models. The robustness of the method is demonstrated by the coherent results obtained for the 10 different cases studied.”
Citation: Stomaci, T., Buonamici, F., Gelati, G., Meucci, F. and Carfagni, M. (2023), "3D-Printed models for left atrial appendage occlusion planning: a detailed workflow", Rapid Prototyping Journal, Vol. 29 No. 11, pp. 74-81. https://doi.org/10.1108/RPJ-10-2022-0351

3D Printing Applications and Workflows: Insights From the Top Ranked US Hospital
Examine real-world case studies of how radiologists have successfully introduced 3D printing capabilities and programs into hospitals.
Clinical Value of Virtual Reality Versus 3D Printing in Congenital Heart Disease
Introduction
“Due to the complex cardiac anatomy and the spectrum of pathologies associated with different types of congenital heart disease (CHD), a complete and scrupulous understanding of the morphology of CHD and the patient’s management is often deemed challenging…. Both three-dimensional (3D) printing and virtual reality (VR) are reported as being superior to the current visualization techniques in conveying more comprehensive visualization of CHD. However, little is known in terms of their clinical value in diagnostic assessment, medical education, and preoperative planning of CHD.”
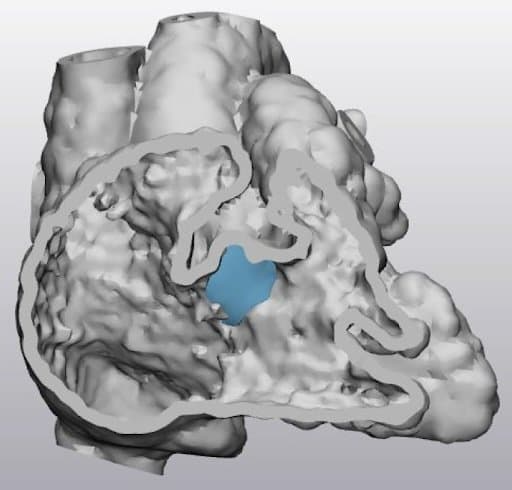
A transected digital heart model demonstrating a ventricular septal defect with a virtual patch (in blue) over the defect.
Materials and Methods
“This cross-sectional study aims to address these by involving 35 medical practitioners to subjectively evaluate VR visualization of four selected CHD cases in comparison with the corresponding 3D printed heart models (3DPHM). Six questionnaires were excluded due to incomplete sections, hence a total of 29 records (1 cardiac radiologist, 1 interventional radiologist, 3 general radiologists, 4 radiology registrars, 3 sonographers, 16 radiographers, and 1 student radiographer) were included for the analysis.”
“The computed tomography angiography (CTA) imaging datasets of four different CHD cases were collected and used as the source data for this project.”
“For 3D printing purposes, the digital heart models were converted into a standard tessellation language (STL) format. The models were printed in polyurethane ... and flexible resin (Flexible V4 Resin, Formlabs, Somerville, Massachusetts, United States), both with shore hardness of 80A."
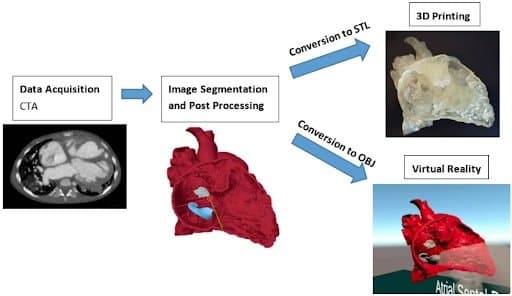
Steps involved in the creation of 3DPHM and the VR project: 3D, three-dimensional; CTA, computed tomography angiography; OBJ, object files; STL, standard tessellation language.
Results and Discussion
“The results showed both VR and 3D printed heart models were comparable in terms of the degree of realism… Twenty-one participants (72%) indicated both the VR and 3DPHM provided additional benefits compared to the conventional medical imaging visualizations.”
“Out of the 29 participants, 22 (76%) indicated both the VR and 3DPHM were helpful to increase surgeons’ confidence for CHD surgeries. No one indicated ‘No’ for this question, suggesting the participants’ positivity towards this aspect.”
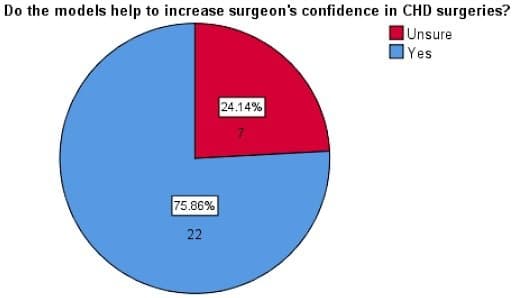
The results show both of them being on a similar level with each other in providing a better visualization experience compared to the conventional visualization technique.
Conclusion
“This study concludes the similar clinical value of both VR and 3DPHM in CHD, although further research is needed to involve more cardiac specialists for their views on the usefulness of these tools.”
Citation: Lau I, Gupta A, Sun Z. Clinical Value of Virtual Reality versus 3D Printing in Congenital Heart Disease. Biomolecules. 2021 Jun 14;11(6):884. doi: 10.3390/biom11060884. PMID: 34198642; PMCID: PMC8232263
Apical Muscular Ventricular Septal Defect Closure via Hybrid Approach Using a Right Ventricular Stay Suture
Introduction
“Apical muscular ventricular septal defects (VSDs) can sometimes be a challenge to close surgically without a ventriculotomy. Their location makes it difficult to reach and visualize through the tricuspid valve from the right ventricular (RV) septal surface. Therefore, a hybrid approach has been used to improve access to the defect, avoid cardio-pulmonary bypass (CPB) and a ventriculotomy. This approach can also decrease morbidity associated with the transvenous transcatheter approach. This report describes a hybrid approach to close a very large apical muscular VSD in an 11 month old with no apical rim using an RV “stay-suture” to prevent device embolization.”
Materials and Methods
“Computed tomography angiography (CTA) demonstrated a 12×14 mm apical muscular VSD. A 3D model was constructed using the end-diastolic images from the CTA, and the blood pool was segmented using ITK-SNAP2 at 1:1 scale. A 1 mm hollow shell was created around the blood pool and printed with part of the ventricular free walls removed on a Form 3 Stereolithography (SLA) Printer (Formlabs Somerville, MA) with Elastic Resin.”
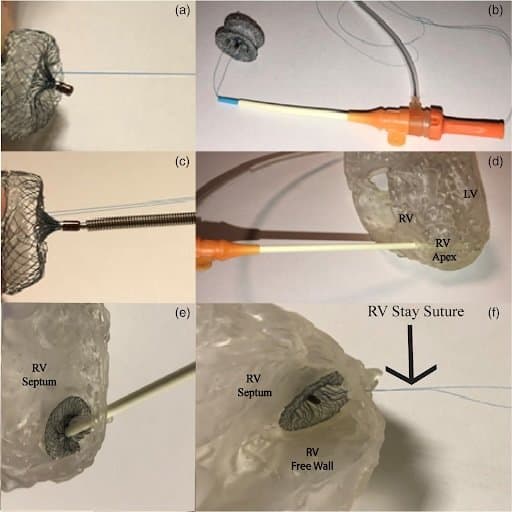
Pre-procedural trial run on a 3D model. (a) Suture through the right ventricular (RV) side of the muscular ventricular septal defect (VSD) device. (b) Suture threaded through the loader. (c) Delivery system attached to muscular VSD device. (d) Sheath advanced into anterior RV wall. (e) Sheath in RV demonstrating RV disc deployed. (f) Device released with stay sutures seen going from the RV disc and out via the anterior RV ready to be secured
Discussion
“Apical muscular VSDs in small children can be difficult to close surgically due to poor direct visualization while percutaneous closure can be limited due to hemodynamic instability related to large sheath manipulation via a wire rail in a small patient. Direct per-ventricular puncture of the RV free wall (hybrid approach) can greatly improve access to the defect and allow for placement of large devices.”
“A 3D model was also manufactured to enhance the understanding and visualization of the patient's anatomy, and augment the decision making for both the interventionist and the surgeon. Furthermore, the 3D model allows for a risk-free environment to rehearse the procedure in order to troubleshoot anticipated difficulties preoperatively. Although it may have been reasonable to attempt a pure transvenous approach, the 3D model further enhanced our decision to proceed with the hybrid approach given the VSD anatomy relative to the patient's size and the desire to anchor the device. The “stay-suture” technique was simulated in the 3D model prior to the procedure. In both the model and the patient, the suture worked well.”
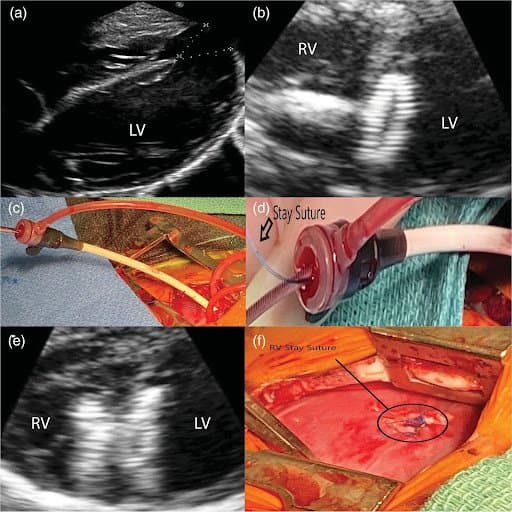
(a) Apical ventricular septal defect (VSD) measurements via transesophageal echocardiogram(TEE) 14 mm×12 mm. (b) Left Ventricle (LV) disc of the device seen released with the delivery system still attached. (c) 9 Fr sheath in the anterior right ventricular (RV) with delivery system. (d) Suture and delivery system visualized going through sheath. (e) TEE of deployed muscular VSD device. (f) Anterior RV stay suture tied to a horizontal mattress autologous pericardial pledgets 5–0 Prolene on the apical surface of the RV.
Conclusion
“A hybrid approach with an RV “stay-suture” guided by a 3D model can be utilized for the closure of large apical muscular VSDs in small patients. This approach may add an additional fail-safe to prevent right-to-left device embolization.”
Citation: Escobar, AJ, Levi, DS, Van Arsdell, GS, Perens, GS, Mohan, UR. Apical muscular ventricular septal defect closure via hybrid approach using a right ventricular stay suture. Catheter Cardiovasc Interv. 2021; 97: E514– E517. https://doi.org/10.1002/ccd.29370
Evaluating 3D-Printed Models of Coronary Anomalies: A Survey Among Clinicians and Researchers at a University Hospital in the UK
Objective
“To evaluate the feasibility of three-dimensional (3D) printing models of coronary artery anomalies based on cardiac CT data and explore their potential for clinical applications.”
Materials and Methods
“Cardiac CT datasets of patients with various coronary artery anomalies (n=8) were retrospectively reviewed and processed, reconstructing detailed 3D models to be printed in-house with a desktop 3D printer (Form 2, Formlabs) using White Resin.”
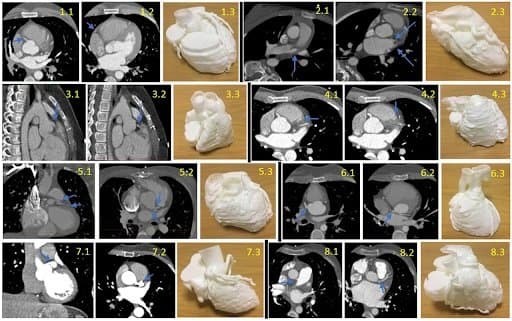
CT Scans and models of each case, with the blue arrows pointing to the abnormality on the CT.
“The CT scans, first, and then 3D-printed models were presented to groups of clinicians (n=8) and cardiovascular researchers (n=9). Models were rated according to clarity of anatomical detail, insight into the coronary abnormality, overall perceived usefulness and comparison to CT scans. Assessment of model characteristics used Likert-type questions (5-point scale from ‘strongly disagree’ to ‘strongly agree’) or a 10-point rating (from 0, lowest, to 10, highest). The questionnaire included a feedback form summarizing overall usefulness. Participants’ imaging experience (in a number of years) was also recorded.”
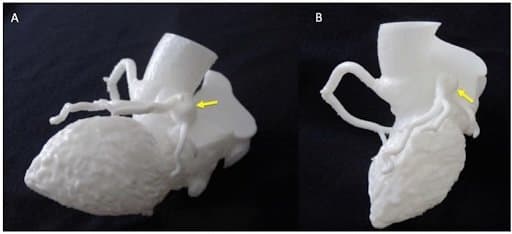
Detail of Kawasaki model for appreciation of coronary aneurysm (indicated by yellow arrows)
Results
“All models were reconstructed and printed successfully, with accurate details showing coronary anatomy (eg. anomalous coronary artery, coronary roofing or coronary aneurysm in a patient with Kawasaki syndrome). All clinicians and researchers provided feedback, with both groups finding the models helpful in displaying coronary artery anatomy and abnormalities, and complementary to viewing 3D CT scans. The clinicians’ group, who had substantially more imaging expertise, provided more enthusiastic ratings in terms of models’ clarity, usefulness and future use on average.”
Detail of ALCAPA model for appreciation of coronary ostium in the pulmonary artery (A) and course of the left coronary artery (B), as indicated by the yellow arrows. ALCAPA, anomalous left coronary artery from pulmonary artery.
Conclusion
“3D-printed heart models can be feasibly used to recreate coronary artery anatomy and enhance understanding of coronary abnormalities.”
Citation: Lee M, Moharem-Elgamal S, Beckingham R, et al, Evaluating 3D-printed models of coronary anomalies: a survey among clinicians and researchers at a university hospital in the UK. BMJ Open 2019;9:e025227. doi: 10.1136/bmjopen-2018-025227

How to 3D Print Anatomical Models for Preoperative Planning and Enhanced Patient Consent
Examine real-world case studies of how radiologists have successfully introduced 3D printing capabilities and programs into hospitals.
The Perception of a Three-Dimensional-Printed Heart Model From the Perspective of Different Stakeholders: A Complex Case of Truncus Arteriosus
Introduction
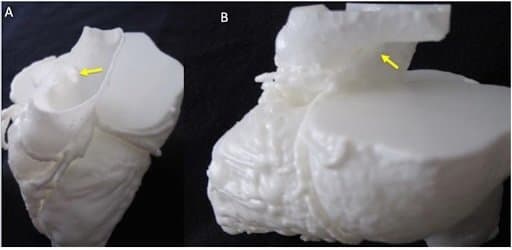
“The case of an 11-year-old male patient with truncus arteriosus is presented. The patient has a right aortic arch, a repaired truncus arteriosus, pulmonary artery stenosis, as well as conduit stenosis, with a complex surgical plan being discussed.”
Methods and Materials
“In order to gather additional insight into the patient’s anatomy prior to the surgery and to facilitate communication with the patient’s parents, a three-dimensional (3D) model of his heart and main vessels was created from computed tomography data. Feedback was collected from different stakeholders.”
“A 3D model was created from computed tomography data… The obtained surface file was further processed using the 3D printer software (PreForm 2.10.3, Formlabs Inc., Somerville, MA, USA), which allowed a scaffold to be automatically created around the model for facilitating the printing process. The model was printed in white resin (Form2, Formlabs Inc.)... The whole process was undertaken at our center, with the 3D printer being available in house.”
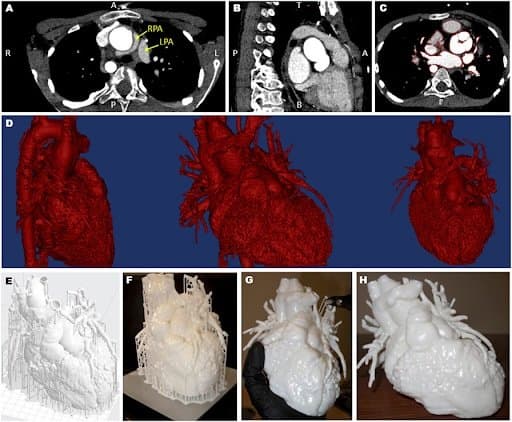
Views of the computed tomography imaging dataset (A–C) including highlight of the position of the left and right pulmonary artery (LPA and RPA), showing the RPA wrapping around the aorta (A); the red outline in panel (C) shows the regions included in the three-dimensional (3D) model; the data are then rendered in 3D [(D), showing different views]; a scaffold (E) is built around the model prior to 3D printing (F) and the removed (G), resulting in the final patient-specific model (H).
Findings: Feedback from Stakeholders
The patient and his parents were both struck by the size of the heart, with the parents further elaborating on how the 3D model was more intuitive a tool than medical images as well as “a helpful talking point to the other members of the family” and potentially also at school. The surgeon and cardiologist commented on gaining a better understanding of the 3D relationship between a markedly narrowed right pulmonary artery and the aorta, with the surgeon ultimately coming to a decision of dividing the ascending aorta quite high to access the right pulmonary artery for patch reconstruction and thus planning to arrest the circulation beforehand. The imaging expert remarked on the potential to “improve communication in multidisciplinary meetings,” while a medical trainee, who also had a chance to evaluate the model, remarked that “having the model in front of me and being able to see the exact abnormality makes this particular case much more memorable. […] 3D printed models could have immense potential in pathology and anatomy teaching for the training of healthcare professionals.”
Conclusion
“…the present report illustrates how an in-house manufactured 3D model was helpful both for the surgeon and cardiologist to gain additional insight into the anatomy prior to the procedure, as well as for the parents and the patient to appreciate key concepts such as the size of the heart, the caliber of the vessels involved in the procedure and their position relative to each other. The feedback collected for this case also highlighted the value of the patient-specific model for improving training and communication among professionals, in agreement with recent observations.”
Citation: Giovanni Biglino, Sarah Moharem-Elgamal, Matthew Lee, Robert Tulloh, and Massimo Caputo. The Perception of a Three-Dimensional-Printed Heart Model from the Perspective of Different Stakeholders: A Complex Case of Truncus Arteriosus. Front Pediatr. 2017; 5: 209. doi: 10.3389/fped.2017.00209
Empowering Innovation in Healthcare
Formlabs continues to expand 3D printing possibilities in medical device and medical component manufacturing as well as at the point of care in hospitals and in medical service bureaus. Biocompatible materials and extensive workflows are designed to support patient care, education, and outcomes.
To discover more about the Formlabs medical printers and materials, or to see further peer-reviewed research, visit our medical page or contact our medical sales team.