Personalized, precision medicine is on the rise. New tools and advanced technologies are bringing doctors closer to patients, delivering treatments and devices customized to better serve each unique individual.
Advances in medical 3D printing technology have made tremendous contributions to fields throughout healthcare. For patients, new tools and therapeutic methods developed through 3D printing can bring new degrees of comfort and personalization to treatment. For doctors, this newly accessible technology allows for a greater understanding of complex cases and provides new tools that can ultimately result in a higher standard of care.
From patient-specific surgical models to 3D printed medical devices, read on to discover six ways 3D printing in healthcare is taking off, why many medical professionals are excited about the potential of 3D printing in the medical field, and how different types of 3D printing technology can be utilized for specific healthcare applications.

Intro to Medical 3D Printing
Join Formlabs for this introduction to learn best practices for medical 3D printing and see the latest Formlabs Medical ecosystem, including multiple new medical-grade products!
3D Printing in Healthcare
1. Patient-Specific Surgical Models
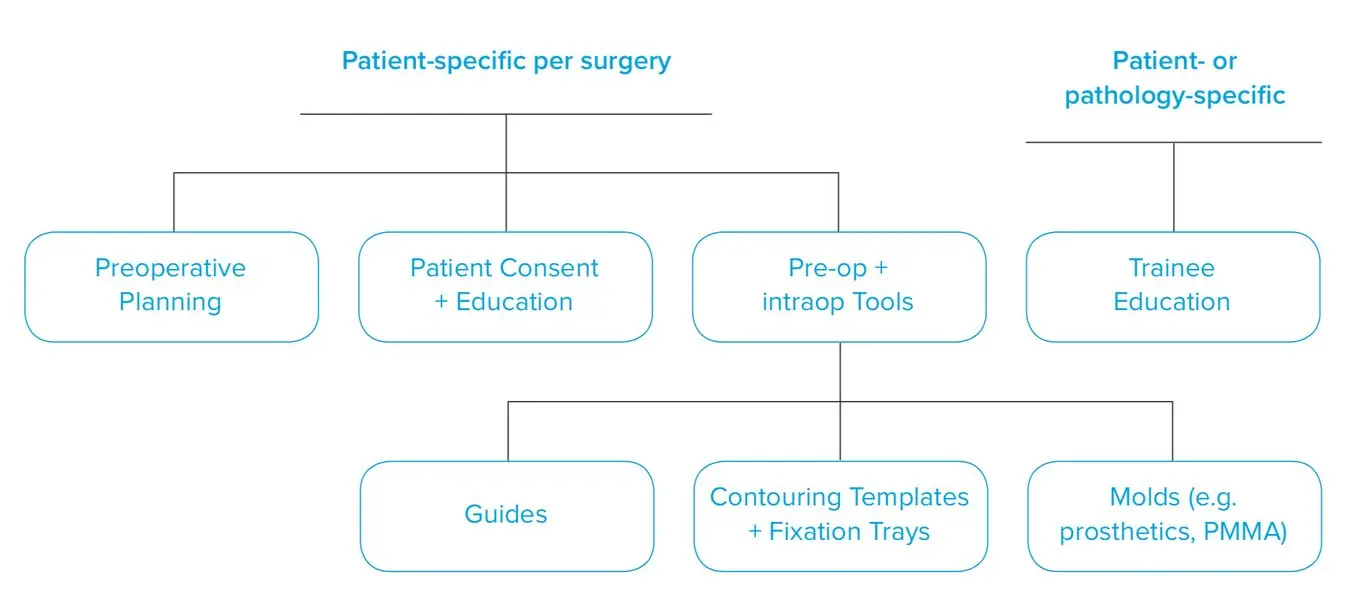
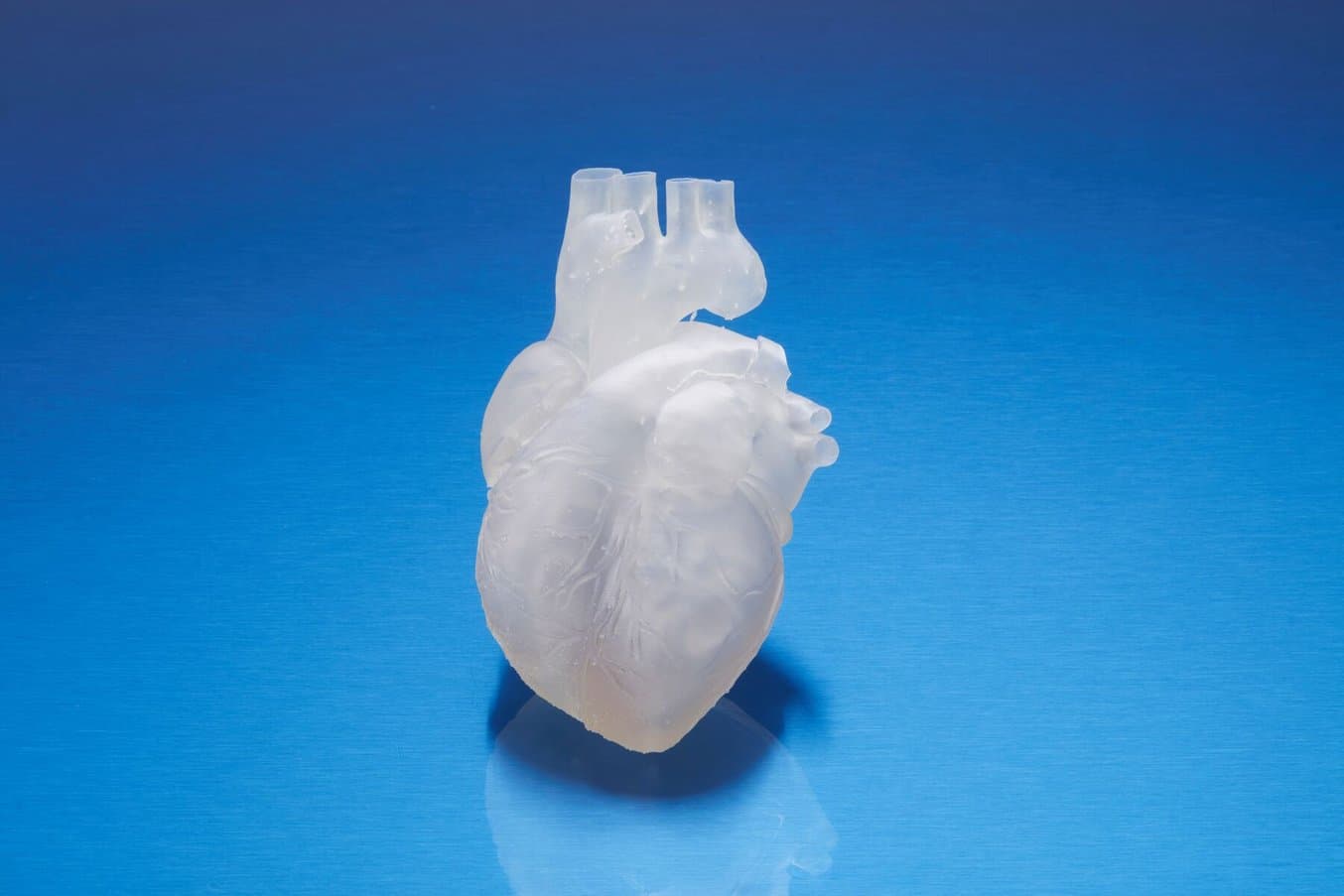
3D printed anatomical models from patient scan data are becoming increasingly useful tools in today’s practice of personalized, precision medicine. As cases become more complex and operating room efficiency becomes more important for routine cases, visual and tactile reference models can enhance understanding and communication within OR teams and with patients.

How to 3D Print Anatomical Models for Preoperative Planning and Enhanced Patient Consent
This white paper offers a practical walkthrough for physicians and technologists to get started creating 3D printed anatomicals models from patient scans, reviewing best practices for setting up a CT/MRI scan, segmenting datasets, and converting files to a 3D-printable format.
Healthcare professionals, hospitals, and research organizations across the globe are using 3D printed anatomical models as reference tools for preoperative planning, intraoperative visualization, and sizing or pre-fitting medical equipment for both routine and highly complex procedures that have been documented in hundreds of publications.
Producing patient-specific, tactile reference models from CT and MRI scans is affordable and straightforward with 3D printing. Peer-reviewed literature shows that they provide an additional view that helps physicians prepare better for surgeries, leading to drastically reduced time and cost in the operating room while improving patient satisfaction, lowering anxiety, and reducing recovery time.

Physicians can use patient-specific surgical models to explain the procedure beforehand, improving patient consent and lowering anxiety.
Learning from preoperative models can influence the course of treatment as well. This was true of the experience of Dr. Michael Eames. After replicating a young patient’s forearm bones, Dr. Eames realized the injury differed from what he’d previously thought.
Dr. Eames settled on a new, soft-tissue procedure — one that was much less invasive, decreased rehabilitation time, and produced far less scarring. Using the printed bone replica, Dr. Eames walked the young patient and their parents through the procedure and obtained their consent.
The result? A surgery time of less than 30 minutes, instead of the initially planned surgery of three hours. This difference in surgery time led to an estimated $5,500 savings for the hospital and meant the patient would need to spend less recovery time in postoperative care.
“Every one of our full-time orthopedic surgeons and nearly all of our part-time surgeons have utilized 3D printed models for care of patients at the San Francisco VA. We’ve all seen that 3D printing improves performance on game day.”
Dr. Alexis Dang, orthopedic surgeon at the University of California San Francisco (UCSF) and the San Francisco Veteran's Affairs Medical Center

Personalized Surgery With 3D Printing: Q&A With Insight Surgery (Formerly 3D LifePrints)
Join this medical 3D Printing Q&A with 3D LifePrints to discover their innovative and versatile work creating patient-specific medical devices.
Dr. Frederik Verstreken at AZ Monica in the Antwerp area of Belgium specializes in hand, wrist, and forearm surgery. He states that the combination of visualization, digital planning, and 3D printed anatomical models empowers clinicians to save around 30-40% of the time in the operating room. For complex osteotomy cases, it was sometimes not possible to restore anatomy. But with 3D printed surgical models doctors come much better prepared to do the operation than without these digital tools, use less radiation, and still achieve substantially higher accuracy, leading to patients regaining normal motion and getting rid of pain.

Anatomical model of a hand, including the 'skin' made out of an elastic 3D printing material.
Todd Goldstein, PhD, Instructor at the Feinstein Institute for Medical Research, is unequivocal in his estimation of how central 3D printing technology has become to his department. He estimates that if Northwell uses 3D printed models in 10-15% of its cases, it could save $1,750,000 a year.
Surgical guides can help surgeons understand each patient’s unique anatomy and pathology, helping them analyze risks, plan an approach, and become more familiar with the case before entering the operating room. Selecting materials for specific properties, such as elasticity, can allow surgeons to practice procedures on models, leading to decreased operating time and better outcomes.
Leveraging Formlabs’ Biocomp Elastomers for Vascular Anatomical Models
Learn how medical professionals can incorporate elastomeric and biocompatible materials into innovative 3D printing workflows using Formlabs’ newest BioMed Flex 80A and BioMed Elastic 50A Resins.
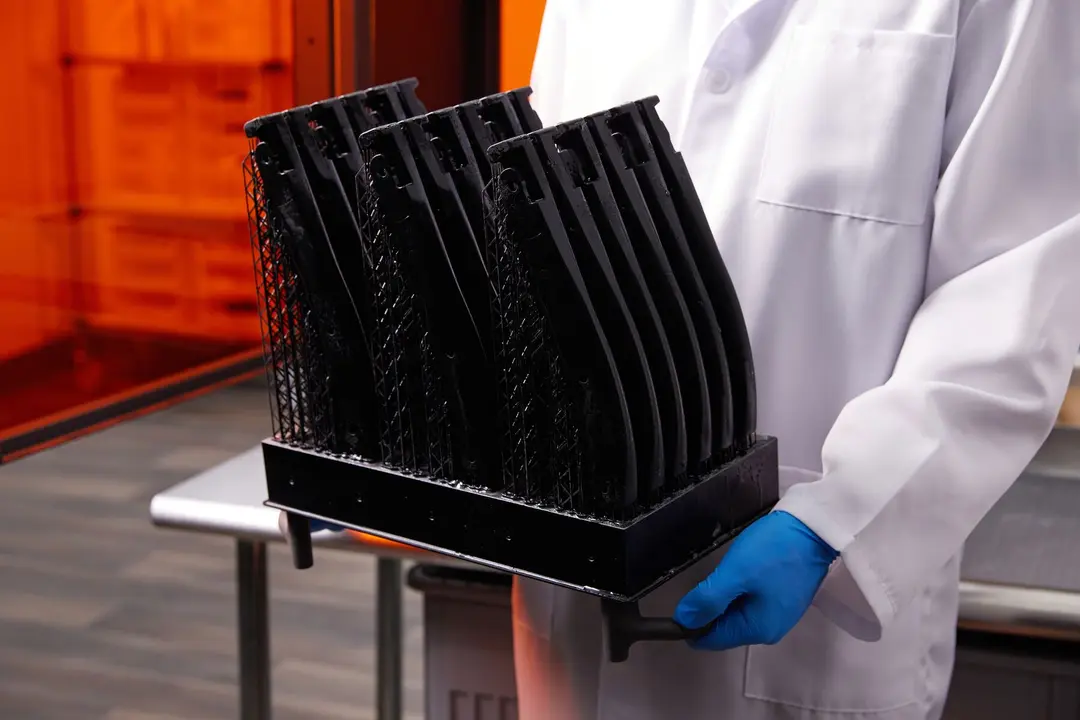
2. Patient-Specific Surgical Instruments
New biocompatible medical 3D printing materials have also enabled new surgical tools and techniques to be developed for the express purpose of further improving clinical experience during surgery. Traditional instrumentation systems are slow to evolve, have significant upfront costs, and often present complications in the surgical workflow. 3D printers and biocompatible materials make it easier and more cost-effective to create procedure-specific and often patient-specific implants, surgical instruments, and cutting guides.
3D printing customized surgical guides can help surgeons understand each patient’s unique anatomy and pathology, helping them analyze risks, plan an approach, and become more familiar with the case before entering the operating room. Well-engineered cutting guides cut down on the time needed for a case and decrease the time surgeons utilize an intraoperative navigation system. This equates to less radiation for the patient, and even less time in the OR.
“The guides tell us where we need to make holes and where we need to make the cuts, so that when we take a plate, everything will fall in the right position. We are much more accurate than without the guides. We save at least 50% of the time with it compared to doing it freehand. And it's much more accurate.”
Frederik Verstreken, Hand and Wrist Surgeon, AZ Monica Hospital
The quick turnaround time of 3D printing allows for quick design iteration. Surgeons can give feedback, which can quickly be applied and the tool or guide reprinted.
restor3d is on a mission to empower surgeons and healthcare providers who repair and reconstruct the human body, driving innovation in precision surgery. restor3d leverages 3D printing capabilities to drastically improve surgical care delivery by printing procedure-specific, and often patient-specific, metal implants and polymer instrumentation.
restor3D has established itself as a leader in using 3D printing to bring innovation to the operating room. Their industry-leading preoperative planning kit, highly accurate and innovative implants, and end-to-end solution provided by the instrumentation kit have helped hospitals reduce costs and improve patients’ experience.
“We get feedback from surgeons constantly. 3D printing allows us to quickly iterate on the design to take surgeons' feedback and deliver a new solution quickly.”
Nathan Evans, Senior Vice President of Product Development, restor3D
Formlabs Biocompatible Resins: A Comprehensive Guide To Choosing the Right Material
Formlabs currently offers more than 40 unique materials for stereolithography (SLA) 3D printing. This paper helps users compare and contrast our biocompatible offerings, and determine the best fit for their medical applications.
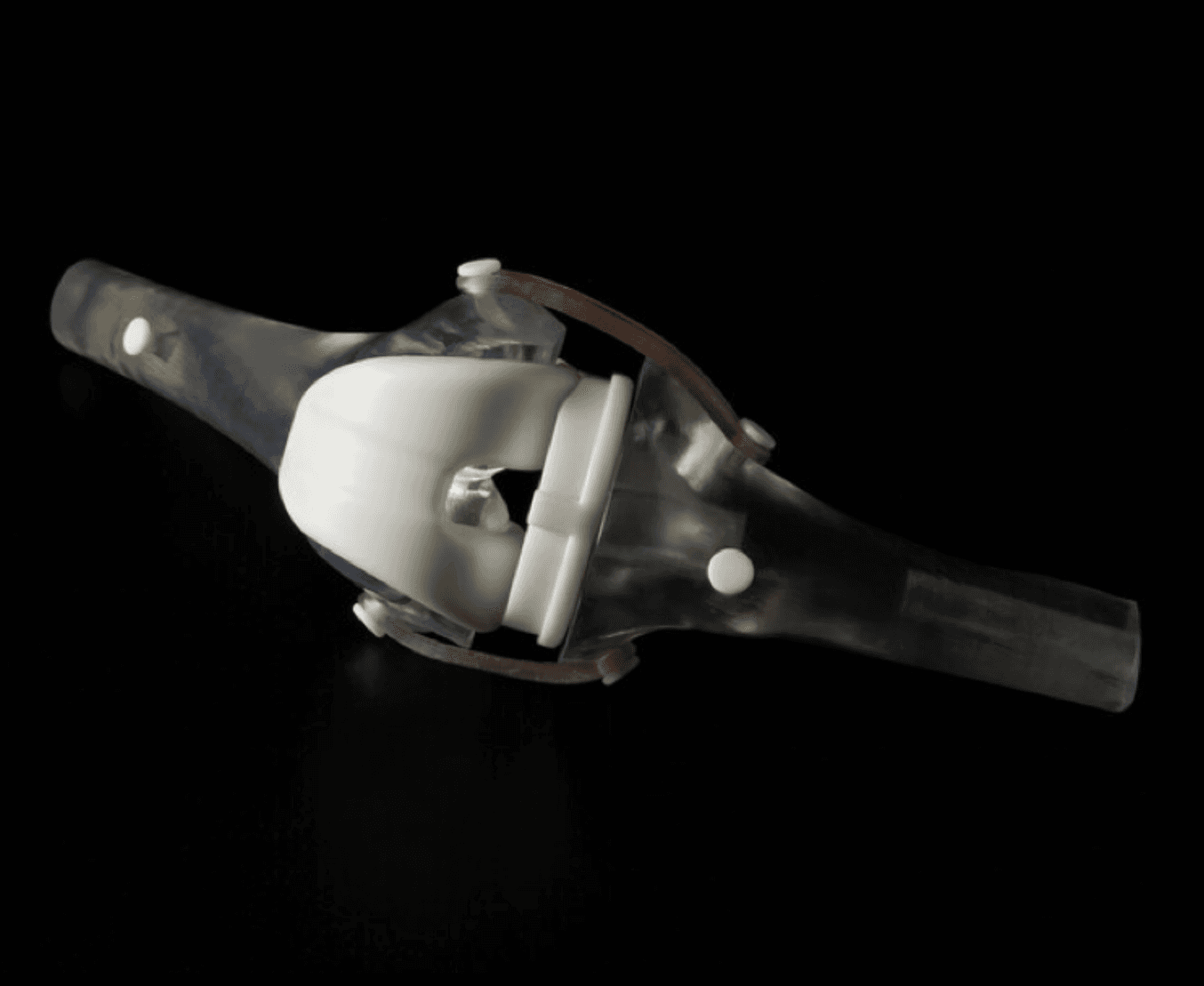
3. New Medical Devices
3D printing has virtually become a synonym for rapid prototyping. The ease of use and low cost of in-house 3D printing have also revolutionized product development and many manufacturers of medical tools have adopted the technology to produce brand new medical devices and surgical instruments.
Over 90 percent of the top 50 medical device companies use 3D printing to create accurate prototypes of medical devices, jigs, and fixtures to simplify testing, as well as directly 3D printing medical devices.

Building a New Medical Device Company with Formlabs Additive Manufacturing
Hear from three inspiring startup companies about their experiences building a brand-new business and simultaneously launching their first medical device. They’ll give us some insight into why they chose Formlabs to be a part of that process and how additive manufacturing was used.
“Before DJO Surgical brought the [Formlabs 3D printer] on board, we relied almost exclusively on outside print vendors for prototypes. Today, we are running four Formlabs machines, and the impact has been profound. Our rate of 3D printing has doubled, cost has been reduced by 70 percent, and the level of print detail allows for clear communication of designs with orthopedic surgeons.”
Alex Drew, a mechanical project engineer at DJO Surgical

Medical device companies like Coalesce use 3D printing to create accurate prototypes of medical devices.
3D printing can accelerate the design process by iterating complex designs in days instead of weeks. When Coalesce was tasked to create an inhaler device that can digitally assess an asthma patient’s inspiratory flow profile, outsourcing to service providers would have resulted in lengthy lead times for each prototype. Design files would have had to be painstakingly refined through various iterations before being sent off-site to be built.
Instead, desktop SLA 3D printing allowed Coalesce to keep the entire prototyping process in-house. The prototypes were fit for use in clinical studies and looked just like a finished product. In fact, when they showcased the device, their clients mistook the prototype for the final product.
Overall, in-house represented an enormous 80-90% reduction in lead time for prototypes. What’s more, the parts took only eight hours to print and could be finished and painted within a few days, while the same process would have taken a week or two through an external contractor.

Creating Silicone Medical Devices
This guide aims to help the user decide on the best method of silicone part production for their intended use, and provides step-by-step instructions for both printing with Silicone 40A, and molding silicone using SLA 3D printed tooling (including two-part injection molds, overmolds, and compression molds).
Shavini Fernando leveraged 3D printing to develop OxiWear, an ear-wearable, vital signs monitoring, and emergency alert accessory. Her team utilized SLA 3D printing to both prototype the device and create static dissipative jigs.
Fernando says, “As a new company just getting started, 3D printing in-house was huge for us, greatly reducing costs over the course of the development lifecycle and it allowed us to test multiple prototype designs simultaneously. Before 3D printing, each time we had to outsource a prototype, it was about $200. Each device prints on the Form 3B for pennies.”
4. Affordable and Advanced Custom Prostheses
Around the world, over 50 million people suffer limb amputation due to traumatic causes. For patients recovering from a medical emergency, entering the new world of prosthetics can be painful. Most want to return to normal life: to drive a car, to workout at the gym, to clean up around the house. But most traditional prosthetic limbs are crude, expensive, and fragile. Approximately 10% of patients requiring an advanced prosthetic arm can afford them today.
Simple prostheses are only available in a few sizes, so patients must make do with what fits best, while custom-fit bionic devices designed to mimic the motions and grips of real limbs that rely on muscles in a person’s residual limb to control their functions are so expensive that they’re only accessible to patients with the best health insurance in developed countries. This particularly affects prostheses for children. As children grow, they inevitably outgrow their prostheses and require expensive replacements. The difficulty is the lack of manufacturing processes that can produce custom parts affordably. But increasingly, prosthetists can take advantage of 3D printing’s much-noted design freedom to mitigate these high financial barriers to treatment.
One company trying to upend the market is PSYONIC, creator of the Ability Hand. Designed and manufactured in-house with hybrid manufacturing methods, the Ability Hand is promising to restore their life, and mobility, back to what it was. PSYONIC utilizes 3D printing to rapidly prototype, increase affordability and access, and create long-lasting end-use parts from durable and impact-resistant materials.
Initiatives such as e-NABLE allow entire communities around the world to form around 3D printed prostheses. They’re driving an independent movement in prosthetic production by sharing information and open-source designs freely online, so patients can get a custom-designed prosthesis that is well-adapted for them for as little as $50.
Other inventors like Lyman Connor, take this one step further. With only a small facility of four desktop 3D printers, Lyman was able to complete and fit his first production prostheses. His ultimate objective? To create a customizable, fully bionic hand to be sold at a fraction of the current tens of thousands of dollars retail price tag for such advanced prostheses.
Elsewhere, researchers at MIT have also identified 3D printing as an optimal means of producing more comfortable prosthesis sockets.
Needless to say, the low cost of producing these prostheses, along with the freedom that comes with custom designs, has proved revelatory. Prostheses made with 3D printing can be turned around in as little as two weeks and then can be trialed and maintained at a much lower cost than their traditional counterparts.
As the costs continue to decrease and material properties improve, 3D printing will undoubtedly play an increasing role in this department of healthcare.

3D Printing in the Orthotics and Prosthetics Industry
This white paper is an introduction to using 3D printing technology to create next-generation orthotics and prosthetic devices.
5. Custom Orthotics
Many of the same high financial barriers to treatment seen in prosthetics are also native to fields such as orthotics. Like many other patient-specific medical devices, custom orthotics are often inaccessible due to their high cost and take weeks or months to get manufactured. With 3D printing, that no longer needs to be the case.
Many healthcare professionals are now adopting 3D printing to produce customized orthopedic solutions. By following tested workflows, 3D printing can save time and resources, allowing for patient-specific orthotics to be produced in record time.
Digital workflows for custom orthotics encompass new design, testing, and manufacturing options to reduce customization costs and speed up production cycles for lower lead times, better-fitting devices, and improved patient outcomes. 3D printed orthotics offer a powerful solution that delivers customization quickly and inexpensively.
Kriwat GmbH, an orthopedic specialist medical provider headquartered in Kiel, Germany, was faced with a shortage of skilled labor. To add to this, traditional workflows created an environment filled with dust and chemical fumes. To address these issues, Lais Kriwat, Master Orthopedic Shoe Technician, developed a digital workflow for insole production using two Fuse 1+ 30W SLS 3D printers and Nylon 11 Powder.
The digital workflow cut out material and labor costs. Lais estimated that the production costs dropped by around 15% to 17%, thanks to 3D printing. It also sped up production enabling workers to take on more patients. “We now have the ability to create a perfect fitting orthotic for a patient within 24 hours,” says Lais Kriwat.
Possibilities enabled by the design freedom of SLS 3D printing include pressure redistribution during walking, individual premium products, certain supports that are not possible to produce with traditional methods, and thinner products that still provide optimal support for the foot for sports like running and football.

3D Printing Rigid Insole Shells Using Fuse 1+ 30W and Nylon 11 Powder
This study investigates material properties and manufacturing methods for custom orthotic insoles: Formlabs Fuse 1+ 30W and Nylon 11 Powder, HP 3D High Reusability PA 11, and traditionally manufactured polypropylene.
Matej and his son Nik are an example of the power of 3D printing custom orthotics. Born prematurely in 2011, difficulties during childbirth caused Nik to have cerebral palsy, a condition that affects almost twenty million people worldwide. Matej was inspired by his son’s unwavering will to transcend the limitations of his condition, but he was faced with a choice between a standard, pre-made orthosis that would have been inadequate and uncomfortable for his son, or an expensive custom solution that would take weeks or months to be delivered, only to be made quickly obsolete by a growing child.
He decided to take matters into his own hands and sought out new solutions to achieve this goal. With the freedom offered by digital technologies including 3D scanning and 3D printing, Matej and Nik's physical therapists were able to experiment liberally and develop an entirely new innovative workflow for ankle foot orthoses (AFOs).
The resulting custom-made, 3D printed orthosis provided Nik with support, comfort, and correction precisely where it was needed, helping Nik to at last take his first independent steps. This custom orthotic device reprised the highly-adjusted finish of high-end orthotics, at a fraction of the price, and with no further adjustments required.
3D printing empowers patient-specific orthotics to be produced with streamlined workflows that save time and resources. For patients, this means fewer appointments, quick turnaround times, and precise customization for increased comfort. Compared to traditional fabrication methods, 3D workflows save time and material resources, while lowering expenses and enabling a more comfortable working environment.
6. Bioprinting, Tissue Engineering, 3D Printed Organs and Beyond
3D bioprinting refers to the use of additive manufacturing processes to deposit materials known as bioinks to create tissue-like structures that can be used in medical fields. Tissue engineering refers to the various evolving technologies, including bioprinting, to grow replacement tissues and organs in the laboratory for use in treating injury and disease.
Researchers are utilizing bioprinting in the development of lab-grown tissues and organs. Achieving these would ultimately advance regenerative medicine and safety testing. Additionally, the ability to bioprint organs could significantly increase the odds of transplant success. Since bioprinting uses cells that are taken from the patient requiring the treatment, it eliminates the possibility of rejection by the immune system — a major issue in conventional organ transplant procedures today.
At Osaka University, researchers have utilized cell-based ink and a printing support to create specific forms including a nose. Once printed, the cells remain viable for up to two weeks, a significant step in the work toward developing lab-grown organs.
Currently, skin regeneration and wound healing are treated via painful skin grafts. The ability to print skin offers an alternative that would promote skin regeneration and wound healing. In 2023, researchers at the Wake Forest Institute for Regenerative Medicine successfully bioprinted full thickness skin that exhibited comprehensive skin healing when transplanted in pre-clinical settings.
Dr. Atala, primary author of the paper, said, "These results show that the creation of full thickness human bioengineered skin is possible, and promotes quicker healing and more naturally appearing outcomes."
Scientists at the Terasaki Institute for Biomedical Innovation have developed a bioink for printing that can enhance the formation of skeletal muscle tissue. Ultimately, the hope is that such technology can be used to help people suffering from muscle loss or injury.
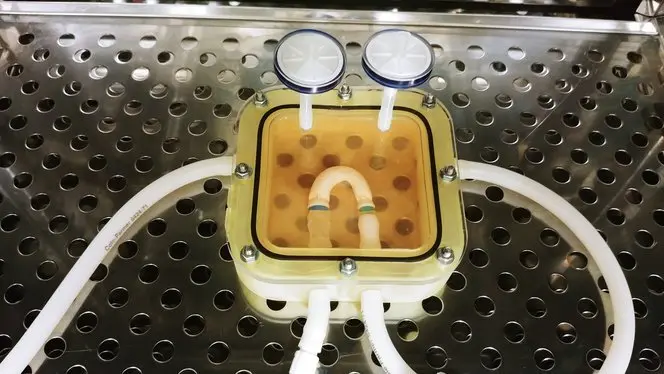
A 3D printed bioreactor chamber with a tissue-engineered miniature aorta growing inside. The tissue is cultured in the bioreactor to acquire the mechanical and biological performance of organic tissue.
3D printing has proven capable of responding to the challenges of producing synthetic blood vessels by solving the difficulties of recreating the precise shapes, sizes, and geometries of the vessel required. Being able to closely match printed solutions to the specific needs of patients has proved revelatory.
In Dr. Pashneh-Tala’s words: “[Creating blood vessels through 3D printing] offers the potential for improved surgical options and even patient-matched blood vessel designs. Without access to high-precision, affordable 3D printing, creating these shapes would not be possible.”
Bioprinting is quickly evolving as researchers push the boundaries of what’s possible. From bones and blood to skin and muscle, developments in bioprinting are setting the stage for future improvements in patient care.
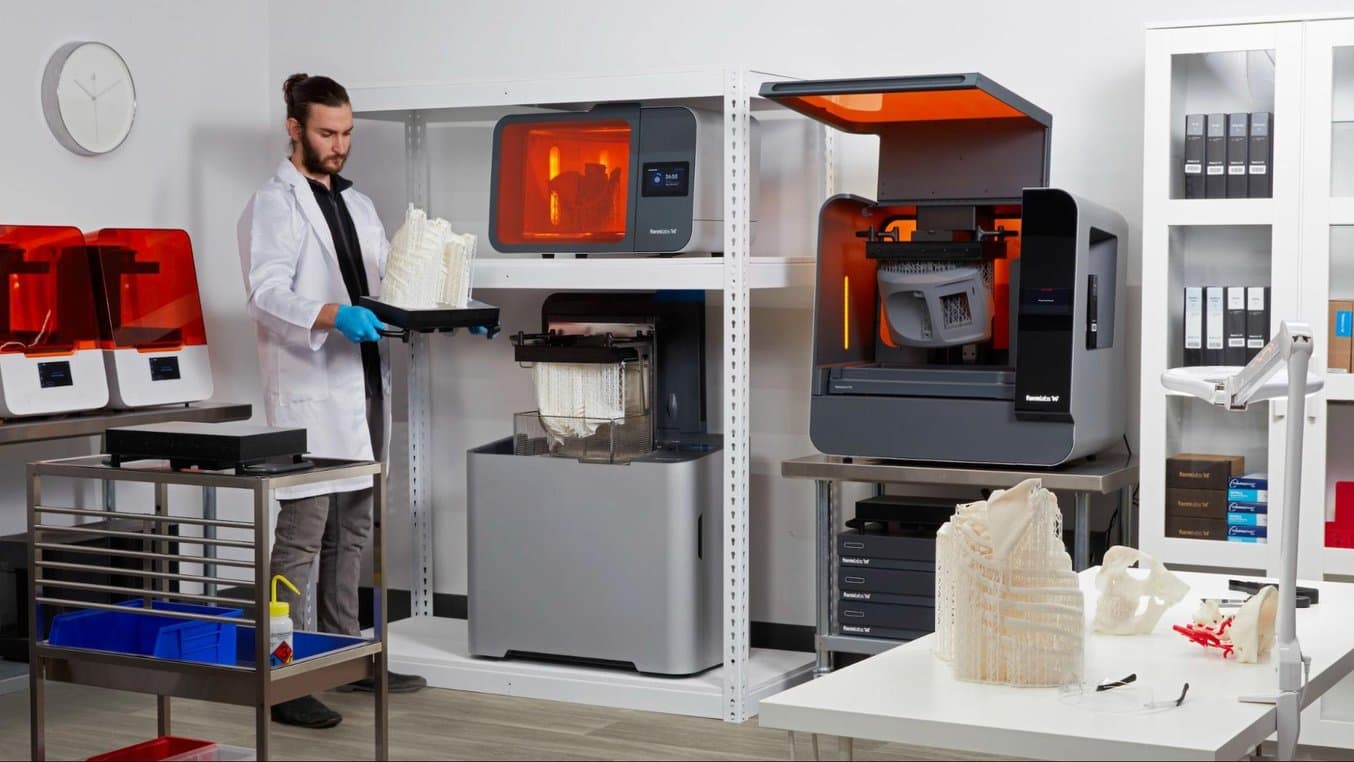
Medical 3D Printing
When it comes to a medical 3D printer, not all methods are created equal. It is important to choose the right printing technology for specific use cases.
The most popular medical 3D printing technologies include stereolithography (SLA), selective laser sintering (SLS), and fused deposition modeling (FDM) for plastic parts, and direct metal laser sintering (DMLS) and selective laser melting (SLM) for metals.
Stereolithography (SLA)
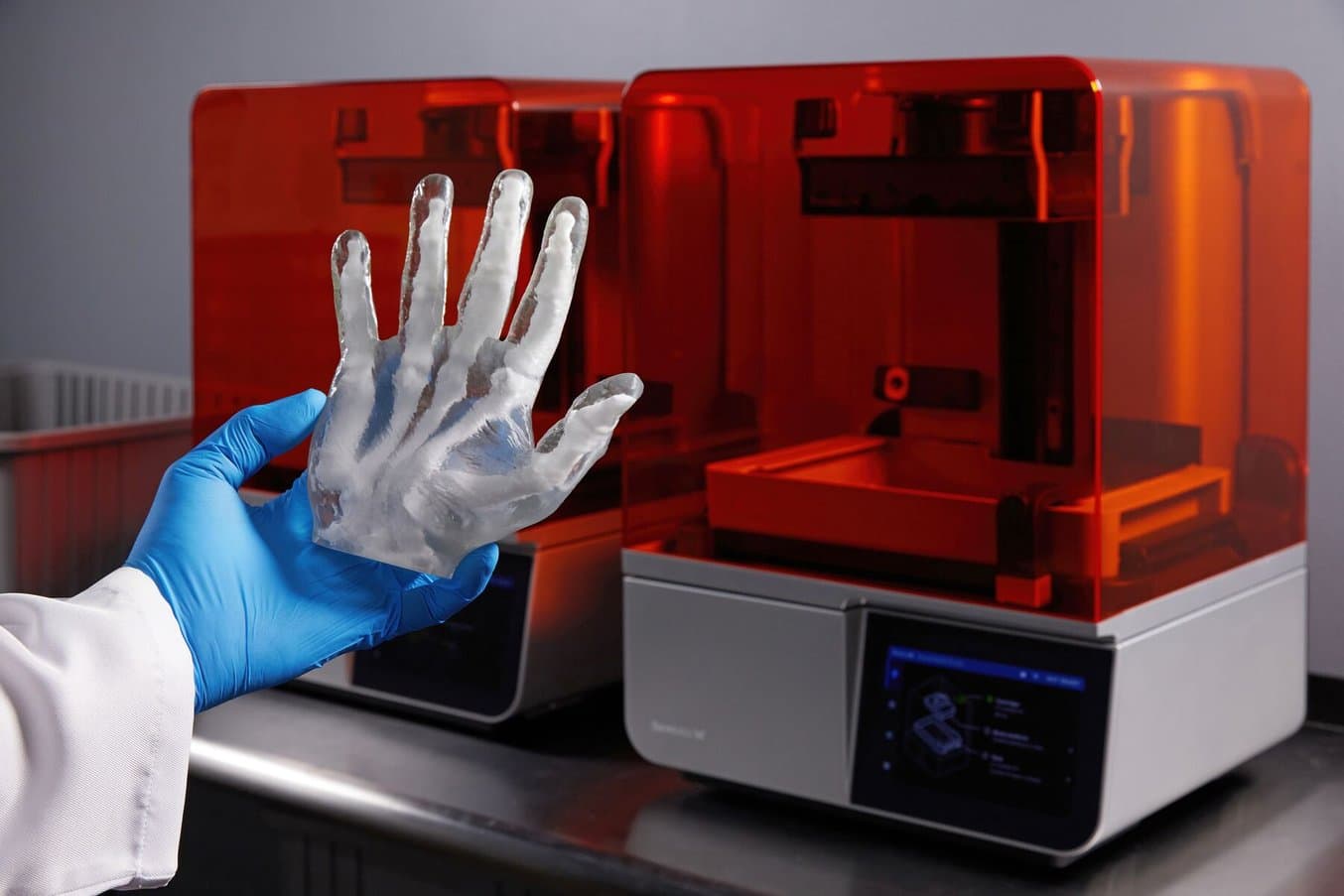
SLA 3D printers use a laser to cure liquid resin into hardened plastic in a process called photopolymerization. SLA is one of the most popular processes among medical professionals due to its high resolution, precision, and material versatility.


SLA 3D printing offers a wide selection of 3D printing materials, including biocompatible materials, for a variety of medical and dental applications.
Advantages of SLA
SLA parts have the highest resolution and accuracy, the clearest details, and the smoothest surface finish of all plastic 3D printing technologies. The main benefit of SLA, however, lies in its versatility. SLA resin formulations offer a wide range of optical, mechanical, and thermal properties to match those of standard, engineering, and industrial thermoplastics.
SLA is a great option for highly detailed anatomical models, medical device prototypes requiring tight tolerances and smooth surfaces, as well as molds, tooling, patterns, and functional end-use parts. SLA also offers the widest selection of biocompatible materials for dental and medical applications, such as surgical instruments and medical appliances requiring skin or mucosal membrane contact.
Disadvantages of SLA
SLA’s wide versatility comes with a slightly higher price tag than FDM, but it is still more affordable than all other 3D printing processes. SLA resin parts also require post-processing after printing, which includes washing the parts and post-curing.

Request a Free Sample Part
See and feel Formlabs SLA quality firsthand. We’ll ship a free sample part to your office.

Formlabs Guide to SLA Quality Control Management for Healthcare Innovators
This guide outlines the steps that healthcare professionals can take to maintain, track and improve the quality of 3D printed SLA parts.

3D Printed Medical Devices for Precision Surgery: Clinical, Commercial, and Regulatory Perspectives
Join Formlabs and Nelson Labs for a deep dive into biocompatibility, including an introduction to our new materials and best practices for medical manufacturers from industry experts.
Selective Laser Sintering (SLS)
SLS 3D printers use a high-powered laser to fuse small particles of polymer powder. The unfused powder supports the part during printing and eliminates the need for dedicated support structures, making SLS a particularly effective choice for complex mechanical parts.
Its ability to produce parts with excellent mechanical capabilities makes SLS the most common polymer additive manufacturing technology for industrial applications. Depending on the material, SLS parts may also be biocompatible and sterilizable, making them ideal for medical devices, prototypes, surgical guides, wearables, and orthotics.
Advantages of SLS
Since SLS printing doesn’t require dedicated support structures, it’s ideal for complex geometries, including interior features, undercuts, thin walls, and negative features. Parts produced with SLS printing have excellent mechanical characteristics, with strength resembling that of injection-molded parts.
The combination of low cost per part, high productivity, established materials, and biocompatibility makes SLS a popular choice among medical device developers for functional prototyping.
Disadvantages of SLS
SLS 3D printers have a higher entry price than FDM or SLA technologies. While a range of materials is available, material selection for SLS is more limited than for SLA. Parts come out of the printer with a slightly rough surface finish and require post-processing such as media blasting for a smooth finish.

SLS 3D printing is ideal for strong, functional prototypes and end-use parts, such as prosthetics and orthotics.

Request a Free Sample Part
See and feel Formlabs SLS quality firsthand. We’ll ship a free sample part to your office.
Fused Deposition Modeling (FDM)
FDM 3D printing, also known as fused filament fabrication (FFF), is a printing method that builds parts by melting and extruding thermoplastic filament, which a printer nozzle deposits layer by layer in the build area.
FDM is the most widely used form of 3D printing at the consumer level, fueled by the emergence of hobbyist 3D printers. Industrial FDM printers are, however, also popular with professionals.
Advantages of FDM
FDM works with an array of standard thermoplastics, such as ABS, PLA, and their various blends. This results in a low price of entry and materials. FDM best suits basic proof-of-concept models and the low-cost prototyping of simpler parts. Some FDM materials are also biocompatible.
Disadvantages of FDM
FDM has the lowest resolution and accuracy when compared to other 3D printing technologies for plastics such as SLA or SLS, which means that it is not the best option for printing complex designs or parts with intricate features, such as anatomical models. Higher-quality finishes require labor-intensive and lengthy chemical and mechanical polishing processes. Some industrial FDM 3D printers use soluble supports to mitigate some of these issues and offer a wider range of engineering thermoplastics, but they also come at a steep price. When creating large parts, FDM printing also tends to be slower than SLA or SLS.
Direct Metal Laser Sintering (DMLS) and Selective Laser Melting (SLM)
Direct metal laser sintering (DMLS) and selective laser melting (SLM) 3D printers work similarly to SLS printers, but fuse metal powder particles together layer by layer using a laser instead of polymers.
DMLS and SLM 3D printers can create strong, accurate, and complex metal products, making this process ideal for a variety of medical applications.
Advantages of DMLS and SLM
The biggest advantage of these processes is obviously the materials, as DMLS and SLM 3D printers are capable of producing high-performing end-use medical devices and components from metal. These processes can reproduce complex geometries and the finished products are strong, durable, and biocompatible. They can be used to manufacture generic implants (hips, knees, spine implants, etc.), custom implants for cancer or trauma treatment, dentures, as well as medical and orthopedic technology products.
Disadvantages of DMLS and SLM
While the prices of metal 3D printers have also begun to decrease, with costs ranging from $200,000 to $1 million+, these systems are still not accessible to most businesses. Metal 3D printing processes also have an involved and complex workflow.
Alternatively, SLA 3D printing is well-suited for metal casting workflows that produce metal parts at a lower cost, with greater design freedom, and in less time than traditional methods.
Compare Medical 3D Printers
| Stereolithography (SLA) | Selective Laser Sintering (SLS) | Fused Deposition Modeling (FDM) | Metal 3D Printing (DMLS, SLM) | |
|---|---|---|---|---|
| Build volume | Up to 300 x 335 x 200 mm (desktop and benchtop 3D printers) | Up to 165 x 165 x 300 mm (benchtop industrial 3D printers) | Up to 300 x 300 x 600 mm (desktop and benchtop 3D printers) | Up to 400 x 400 x 400 mm (large industrial DMLS/SLM) |
| Price range | Professional desktop printers start at $2,499, large-format benchtop printers at $8,999, and large-scale industrial machines are available from $80,000. | Benchtop industrial systems start at $24,999, and traditional industrial printers are available from $100,000. | Budget printers and 3D printer kits start at a few hundred dollars. Higher quality mid-range desktop printers start around $2,000, and industrial systems are available from $15,000. | Starting from $200,000. |
| Materials | Varieties of resin (thermosetting plastics). Standard, engineering (ABS-like, PP-like, flexible, heat-resistant), castable, dental, and medical (biocompatible). Pure silicone and ceramic. | Engineering thermoplastics (including biocompatible materials). Nylon 11, nylon 12, glass or carbon-filled nylon composites, polypropylene, TPU (elastomer). | Standard thermoplastics, such as ABS, PLA, and their various blends. | Stainless steel, tool steel, titanium, cobalt chrome, and aluminum. |
| Ideal applications | Anatomical models (biocompatible), surgical instruments (biocompatible), medical devices (biocompatible), dental appliances (biocompatible), rapid prototyping, rapid tooling, manufacturing aids, and end use parts. | Anatomical models (biocompatible), surgical instruments (biocompatible), medical devices (biocompatible), orthotics and prosthetics, rapid prototyping, rapid tooling, manufacturing aids, and end use parts. | Basic proof-of-concept models. Low-cost prototyping of simple parts. | Strong, durable parts with complex geometries, implants, dentures, medical and orthopedic components out of metal. |
Materials for Medical 3D Printing Applications

The Formlabs material library includes resins for SLA printing and powders for SLS printing optimized for a variety of medical applications.

Material Mastery for 3D Printing Medical Devices
In this webinar, Formlabs Medical Engineer Shiden Yohannes explores the diverse materials available for 3D printing and their unique properties, guiding you to make informed choices for your specific needs.
Resins for SLA
SLA supports a wide range of applications including engineering, manufacturing, and healthcare. Resins for SLA have been developed with specific material properties, including options that are elastic, durable, and biocompatible.
For healthcare professionals, Formlabs BioMed Resins are medical-grade materials for a wide range of applications where performance and biocompatibility are critical. Materials in the BioMed Resin family are developed and manufactured in an ISO 13485 certified facility and are compatible with common disinfection and sterilization methods.
Selecting the appropriate resin depends upon the application, mechanical requirements of the material, and the use case. Formlabs BioMed Resins include both rigid and elastic options, including some for long-term or mucosal membrane contact.
Additionally, a library of materials has been developed specifically to meet the needs of dental professionals. Resins include Premium Teeth Resin for the direct printing of denture teeth, and Dental LT Comfort Resin for occlusal splints. A full catalog of materials and information about the 17+ applications for Formlabs’ Dental Resins, are available on Formlabs Dental.

Formlabs Resins specially formulated for the dental market can be used to print over 17 dental applications.
Diversifying the types of medical resins helps healthcare professionals with an array of important tasks: creating medical devices, planning surgical procedures, developing custom implants, and conducting research. BioMed resins provide healthcare professionals with a variety of material options, expanding 3D printing capabilities. The table below compares Formlabs BioMed resin properties and applications.
| Material | Description | Applications |
|---|---|---|
| BioMed White Resin | Rigid and opaque white. Approved for long-term skin (>30 days) or short-term bone, tissue, dentin, and mucosal membrane contact (<24 hours). | End-use medical devices and device components; patient-specific implant sizing models and molds; cutting and drilling guides; surgical tools and templates; biocompatible molds, jigs, and fixtures; anatomical models that can be used in the OR. |
| BioMed Black Resin | Rigid and matte black. Approved for long-term skin (>30 days) and short-term mucosal membrane contact (<24 hours). | Medical devices and device components; biocompatible molds, jigs, and fixtures; end-use parts requiring patient contact; consumer goods. |
| BioMed Amber Resin | Rigid and semi-transparent. Approved for long-term skin (>30 days) or short-term bone, tissue, dentin, and mucosal membrane contact (<24 hours). | End-use medical devices; implant sizing models; cutting and drilling guides. |
| BioMed Clear Resin | Rigid and transparent. Approved for long-term skin (>30 days), breathing gas pathways, and mucosal membrane contact (>30 hours) or short-term bone, tissue, and dentin (<24 hours). | End-use devices, including gas pathway devices; biocompatible prototypes, molds, jigs and fixtures; models for visualization and implant sizing; cell culture and bioprocess devices. |
| BioMed Durable Resin | Impact, shatter, and abrasion resistant. Transparent. Approved for long-term skin (>30 days) and mucosal membrane (>30 hours) or short-term tissue, bone, and dentin contact (<24 hours). | Patient-specific instruments; single-use instruments; end-use devices and components requiring biocompatibility and impact resistance. |
| BioMed Elastic 50A Resin | Soft and silicone-like. Translucent. Approved forlong-term skin (>30 days) or short-term mucosal membrane contact (<24 hours). | Comfortable medical devices requiring long-term skin contact; biocompatible soft tissue models surgeons can reference in the operating room. |
| BioMed Flex 80A Resin | Hard rubber-like. Translucent. Approved for long-term skin (>30 days) or short-term mucosal membrane contact (<24 hours). | Flexible biocompatible medical devices and components; medical devices requiring short-term mucosal membrane contact; firm tissue models to assist in surgeries. |
Creating Bone Simulation Models for Cutting and Drilling
3D printed bone-simulation models are revolutionizing medical training, surgical planning, research, and medical device development. This application guide walks through the bone-simulation material options for stereolithography (SLA) 3D printing and the entire in-house manufacturing process for bone-like anatomical models intended for cutting and drilling.
Powders for SLS
SLS powders can be biocompatible, skin-safe, and sterilizable, and designs can have fine details and thin walls. These properties make them ideal for healthcare applications including medical devices, prototypes, prosthetics, surgical instruments, and orthotics.
The most common material for SLS is nylon, a popular engineering thermoplastic with excellent mechanical properties. Nylon is lightweight, strong, and flexible, as well as stable against impact, chemicals, heat, UV light, water, and dirt. 3D printed nylon parts can also be biocompatible and not sensitizing, which means that they are ready to wear and safe to use in many contexts.
Nylon 12 Powder balances strength and detail with a tensile strength of 50 MPa. Capable of complex assemblies and durable parts with high environmental stability, Nylon 12 Powder is ideal for high performance prototyping, low volume manufacturing, and permanent jigs, fixtures, and tooling. Parts are biocompatible and sterilizable, making Nylon 12 ideal for medical applications, such as surgical guides.
Nylon 11 Powder is an ideal material for tough orthotics with high ductility and long-term stability, including insole shells. Learn more about the durability of this material in this performance analysis.

Orthotics printed with Nylon 11 Powder.

A cranial remolding helmet and a prototype of a prosthetic printed with TPU 90A Powder.
Genuine Polypropylene Powder can be leveraged to produce works-like prototypes and durable end-use parts. Offering high ductility, it allows for repeated bending and flexing while ensuring durability. Parts printed with Polypropylene Powder are chemically resistant, weldable, and watertight, making them ideal for orthotics, prosthetics, fixtures, tools, and jigs.
TPU 90A Powder is a flexible elastomer combining the high tear strength and elongation at break of rubber materials with the design freedom and durability of SLS 3D printing. TPU, or thermoplastic polyurethane, is a commonly used elastomeric thermoplastic. In orthotics, this skin-safe material is often used for medical device prototypes and end-use medical devices and components, orthotic pads and prosthetic liners, splints, cranial remolding helmets, and athletic and corrective insoles.
The table below breaks down some of the material properties and applications for Formlabs’ SLS powders.
| Material | Description | Applications |
|---|---|---|
| Nylon 12 Powder | High tensile strength and durability, biocompatible, sterilizable. | End-use medical devices and device components; patient-specific implant sizing models and molds; cutting and drilling guides; surgical tools and templates; biocompatible molds, jigs, and fixtures; anatomical models that can be used in the OR. |
| Nylon 11 Powder | Highly ductile and robust. More flexible, less brittle and better at printing thin walls than Nylon 12. Biocompatible, sterilizable. | Orthotics and prosthetics, impact resistant prototypes, medical devices, end-use parts. |
| Polypropylene Powder | Ductile and durable, chemically resistant, watertight, weldable. | Orthotics and prosthetics, watertight housings and cases, strong and chemically resistant fixtures, tools, and jigs. |
| TPU 90A Powder | Tough elastomer, skin-safe, resilient to deformation, high elongation at break and superior tear strength. | Soles, splints, orthotics, and prosthetics. Wearables and soft-touch elements. Padding, cushions, and grippers. |
Material properties may vary based on part design and manufacturing practices. It is the manufacturer’s responsibility to validate the suitability of the printed parts for the intended use.

3D Printing Rigid Insole Shells
Learn how to produce strong, ductile insole shells exceeding 4 million bend cycles with Formlabs’ compact, affordable SLS ecosystem. This comprehensive guide will help you hit the ground running with insole shell production on the Fuse 1+ 30W.
Get Started With Medical 3D Printing
Precise and affordable medical 3D printing processes are democratizing access to the technology, empowering healthcare professionals to develop new clinical solutions and quickly manufacture custom devices, and allowing physicians to deliver new treatments across the globe. As medical 3D printing technologies and materials continue to improve, they will pave the path for personalized care and high-impact medical applications.
Every medical facility should have access to the latest tools to improve care and provide the best patient experience. Get started now or expand your in-house production with Formlabs, a proven, cutting-edge partner in medical 3D printing.
Reach out to our medical experts to learn more about how in-house 3D printing can provide better treatment and supplement your current medical device design and manufacturing workflow.